Anti-inflammatory diet and cognitive impairment: role of the oral and gut microbiota
Anti-inflammatory diets support a healthy oral and gut microbiota, leading to better cognitive performance... and perhaps helping prevent cognitive decline?
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
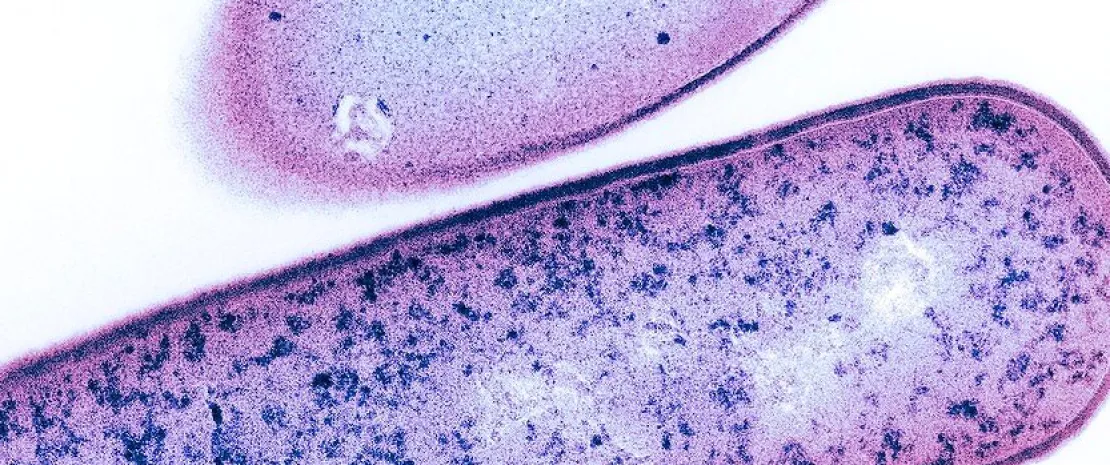
Roughly one in six Chinese adults over 60 experience (sidenote: Mild Cognitive Impairment (MCI) MCI is a clinical stage between the expected cognitive decline of normal aging and the more severe decline of dementia. Individuals with MCI have noticeable memory or thinking problems but can still perform most daily activities, representing a critical window for intervention and study. ) , with an annual risk of progression to dementia of 6 to 15% (10 times higher than in people without MCI). How can we act at this stage? Through diet, according to a study that assessed how the inflammatory potential of the diet affects the diversity and composition of the oral and gut microbiota, as well as cognitive performance, in 54 Chinese adults over 60 (36 with MCI and 18 controls without).
15.54% The prevalence of mild cognitive impairment (MCI) among older Chinese people > 60 years of age is approximately 15.54%.
10x The annual conversion rate to dementia ranges from 6 to 15% for Chinese MCI patients, which is about 10 times higher than the conversion rate for cognitively normal older adults.
Diet affects oral diversity
Oral microbiota diversity varies according to the dietary inflammatory score (measured by the
(sidenote:
E-DII score (Energy-adjusted Dietary Inflammatory Index)
An epidemiological tool designed to assess an individual’s overall dietary inflammatory potential by adjusting this score according to total caloric intake, allowing standardized comparison between individuals regardless of energy consumption.
)
); oral microbial richness (measured by the Shannon index) decreases as the inflammatory potential of the diet increases.
However, the inflammatory score does not seem to significantly affect gut microbiota diversity.
Altered microbiota
Microbiota composition also changes. In individuals with an anti-inflammatory diet (tertile T1), the oral abundance of certain bacteria increases 1. Among those following pro-inflammatory diets (T3), the most enriched taxa belong to the genus Lacticaseibacillus.
As for the gut microbiota, two taxa (the family Porphyromonadaceae and its genus Porphyromonas) were more abundant with a pro-inflammatory diet, while some bacteria (including the genera Haemophilus, Holdemanella, and norank.RF39) show reduced abundance.
Associations with cognitive functions
Finally, the authors highlight links between microbiota and cognitive performance (memory, language, attention). For example, in the oral cavity, 3 bacteria typical of anti-inflammatory diets 1 were associated with higher test scores, while the genus Lacticaseibacillus (inflammatory diet) correlated with poorer performance. How can these effects be explained? Eubacterium produces butyrate, a brain-protective anti-inflammatory fatty acid. Lactobacillaceae synthesize acids that cause cavities and systemic inflammation.
In the gut microbiota, the bacterium Haemophilus (inflammatory diet) appears linked to poorer performance, while two other digestive microorganisms, Holdemanella and Porphyromonas, show positive associations with cognition.
A pro-inflammatory diet may alter gut microbiota composition and trigger an inflammatory response in peripheral circulation and in the central nervous system through a two-way “microbe–gut–brain” communication axis, which could impair cognitive brain function.
Predicting cognitive decline?
Distinct oral and gut microbiota profiles could indicate the onset of disorders. Artificial intelligence models can predict mild cognitive impairment based solely on these microbiota, with moderate accuracy for the oral microbiota (
(sidenote:
AUC (Area Under the Curve)
A measure of a model’s ability to correctly distinguish between two classes (for example, “diseased” vs “healthy,” “positive” vs “negative”). It represents the area under a curve that plots the true positive rate (sensitivity) on the y-axis against the false positive rate on the x-axis. If the AUC equals 1, the model performs perfectly; above 0.80 it is generally considered very good, and above 0.90, excellent; at 0.5, it performs no better than random chance.
)
= 0.75) and high accuracy for the gut microbiota (AUC = 0.87).










