How oral microbiome metabolites drive gum disease & inflammation
What if gum disease isn't just about oral bacteria, but what they secrete? A new study 1 reveals specific oral microbiome metabolites that don’t just coexist, they inflame, damage, and drive periodontal disease. The mouth may speak, but the metabolites scream.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Author
Periodontal diseases (gum diseases) represent a major global health concern. A significant contributing factor to their development and progression is (sidenote: Dysbiosis Generally defined as an alteration in the composition and function of the microbiota caused by a combination of environmental and individual-specific factors. Levy M, Kolodziejczyk AA, Thaiss CA, et al. Dysbiosis and the immune system. Nat Rev Immunol. 2017;17(4):219-232. ) of the oral microbiota. Historically, we've focused heavily on identifying pathogenic species of bacteria, but this new study 1 shines a spotlight on another critical layer: the metabolites these microbes produce, and how they directly influence the health of our gum tissues.
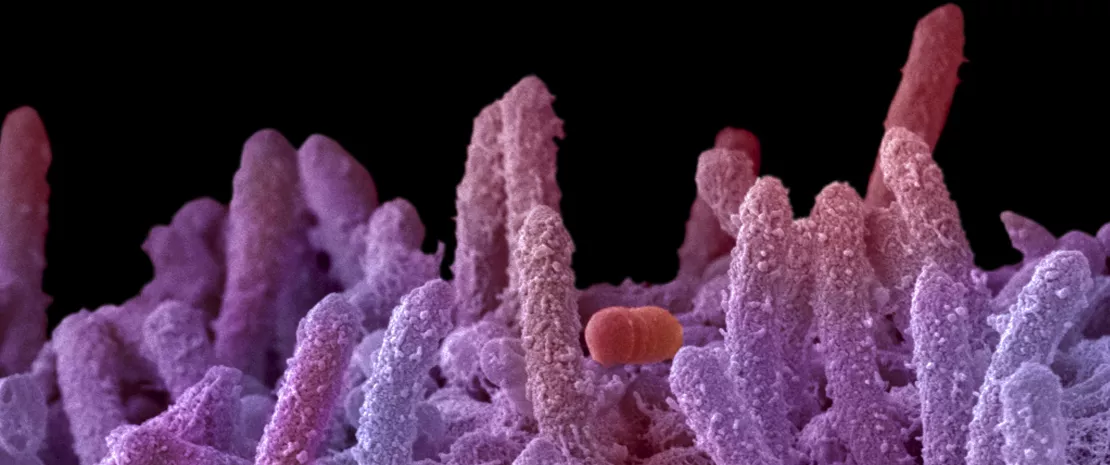
The study shows that the imbalance in the oral microbiota directly affects the quantity and compositional balance of metabolites. Some metabolites correlated with bacteria prevalent in periodontitis can exhibit inflammation-inducing effects on human (sidenote: Gingival epithelial cells These are the surface cells that form the lining of the gums and act as the first barrier against microbial invasion in the oral cavity. ) . This demonstrates a clear link between the altered oral microbial ecosystem, its metabolic output, and the inflammatory response in the host tissues.
Microbiome-metabolite connection
The authors, from Kyushu University Faculty of Dental Science, Japan, examined mouth-rinsed water from individuals with periodontal disease (n=24) and healthy controls (n=22). Mouth-rinsed water is considered an appropriate sample as it reflects information present in saliva. They didn't just identify the bacteria more prevalent in disease states, confirming the usual suspects like Porphyromonas gingivalis and Fusobacterium nucleatum, but crucially, they correlated these specific bacterial species with the metabolites found in the same samples. This targeted approach identified 20 metabolites strongly associated with the periodontitis microbiome. These weren't just random compounds; they included things like amino acid derivatives, (sidenote: Short chain fatty acids (SCFA) Short chain fatty acids (SCFA) are a source of energy (fuel) for an individual’s cells. They interact with the immune system and are involved in communication between the intestine and the brain. Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. ) , and polyamines.
This approach highlights how deeply the oral microbiome interacts with the host environment through its metabolic byproducts. In addition to well-known bacterial species, the study demonstrates that their metabolic profiles — especially under disease conditions — can significantly disrupt plaque homeostasis, suggesting that such imbalances are not just correlative but possibly causal.
Metabolites with pathogenic effects
The next critical step was to see if these identified metabolites could actually do something to human gum cells. They tested 20 correlated metabolites on human gingival epithelial cells. The results showed that several compounds exhibited clear signs of pathogenicity. Specifically, propionate, succinate, (sidenote: Homoserine An amino acid derivative not commonly found in human metabolism but produced by certain bacteria; it may have pro-inflammatory or cytotoxic effects on host tissues like gum epithelium. ) , and citrulline significantly inhibited the growth of these gum epithelial cells. Furthermore, treating cells with homoserine, propionate, and succinate significantly ramped up the expression of (sidenote: Interleukin-8 (IL-8) A signaling protein (cytokine) released by cells to attract immune cells like neutrophils to the site of infection or inflammation; elevated IL-8 often indicates ongoing tissue inflammation. ) , a key inflammatory cytokine, indicating these metabolites can trigger local inflammation and contribute to plaque-induced tissue damage.
The study also suggests that chronic periodontitis may be exacerbated by a sustained imbalance in microbial metabolism, making microbial metabolites potential biomarkers of both early disease onset and plaque disruption.
Finally, while homoserine was known to be produced by other bacteria, this study presented a new finding by detecting its production by several key periodontal bacteria species, including Prevotella melaninogenica, Prevotella intermedia, and Porphyromonas gingivalis. This suggests these periodontitis-associated microbes are directly contributing to the local homoserine levels observed in diseased states confirming their host-impacting potential.
Solutions for gum diseases?
New dental microbiome-based therapies are offering promising alternatives for treating gum disease by restoring a healthy balance of microbial communities in the mouth. Probiotics, beneficial bacteria found in supplements, have been shown to reduce inflammation and harmful microbes when used alongside traditional dental care.
Other innovative and emerging approaches, such as oral microbiome transplants 2 and targeted antimicrobial peptides, are being explored in research settings, with the goal of providing gentler, more effective treatments that address the root cause of gum disease rather than simply eliminating all bacteria.
In essence, this study provides compelling evidence that specific metabolites, beyond the bacteria themselves, are active participants in driving periodontal disease progression. These microbial byproducts offer new therapeutic targets and may also serve as novel diagnostic indicators of periodontitis, opening up future perspectives in predictive care, oral diagnostics, and microbiota-centered therapy.













