Cancer: microbiota involved in the abscopal effect
What explains the abscopal effects of radiotherapy during immunotherapy? Low-dose gut irradiation, whether intentional or accidental, appears to act in synergy with immunotherapy, with the gut microbiota playing a major role.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
The (sidenote: Abscopal effect From Latin ab-, “away from”, and Greek skopos, “target,” lit. “away from target” - Regression of tumor lesions located outside the field of irradiation when irradiation of a lesion activates antitumor immune responses or enhances their effectiveness, thereby leading to the destruction of non-irradiated lesions by antitumor immune effectors. Explore https://doi.org/10.1016/j.mednuc.2024.11.007 ) effects of radiotherapy are one of the mysteries of cancer research, observed in some patients but not in others. However, in 2025, an international team made a major breakthrough, showing that intestinal low-dose irradiation (ILDR) increased the clinical benefits of chemotherapy and immunotherapies that target (sidenote: Immune checkpoints are used by tumors to protect themselves from immune system attacks and may be blocked by ICI therapy in order to restore the immune system function. ) , in eight retrospective patient cohorts and a preclinical murine model. This research highlights the key role of the gut environment in treatment response.
A matter of dose...
The researchers’ starting point was patients with metastatic tumors in a phase 2 multicenter trial who received (sidenote: Stereotactic ablation radiotherapy (SABR), also known as stereotactic body radiation therapy (SBRT) Is radiotherapy based on the emission of numerous radiation beams from different angles that converge on the tumor. The tumor therefore receives a high dose of radiation, while beams that pass through the surrounding tissue are low-dose. This reduces the effects of radiation on the healthy tissue surrounding the tumor. SBRT is administered in fewer sessions than standard external radiation therapy. SBRT can be used to treat tumors in the pancreas, lungs, liver, or spine. Explore https://cancer.ca/fr/treatments/treatment-types/radiation-therapy/external-radi… ) in combination with an anti-PD-L1 antibody. Among them, 13 patients (41%) exposed to accidental ILDR, with a median radiotherapy dose of 3.3 Gy to the duodenum, 1.0 Gy to the jejunum/ileum, and 1.3 Gy to the colon, showed a much better 24-month survival rate of 38% (5/13) versus 5% (1/19). This highlights the increased efficacy of combination therapy.
Treatment with ILDR at 1 Gy alone did not improve survival, while anti-PD-L1 alone had only transient effects (relapse). However, combining ILDR at 1 Gy with anti-PD-L1 cured 30% of animals, unlike lower (0.25 Gy) or higher (4 Gy) doses, which did not cure any mice. This shows that the effectiveness of treatment depends on a precise synergy between radiation dose, immunotherapy, and immune cells.
Microbiota, cancer, and immunotherapy
The gut microbiota plays a key role in the response to cancer immunotherapy. Certain gut bacteria, such as those from the Clostridiales order, strengthen anti-tumor immunity. Conversely, antibiotics can compromise the effectiveness of immune treatments. Fecal microbiota transplantation (FMT) is thus emerging as a promising therapeutic strategy.
... and bacteria
The anti-tumor immune response and survival also appear to be linked to differences in gut flora between individuals: compared to healthy adults, non-responders to treatment combining ILDR and anti-PD-L1 antibodies harbored – prior to treatment – fewer species of bacteria typical of responders (Christensenella minuta and Ruminococcus bromii) and more species of bacteria typical of a poor response to treatment (Enterocloster aldensis and Parabacteroides distasonis).
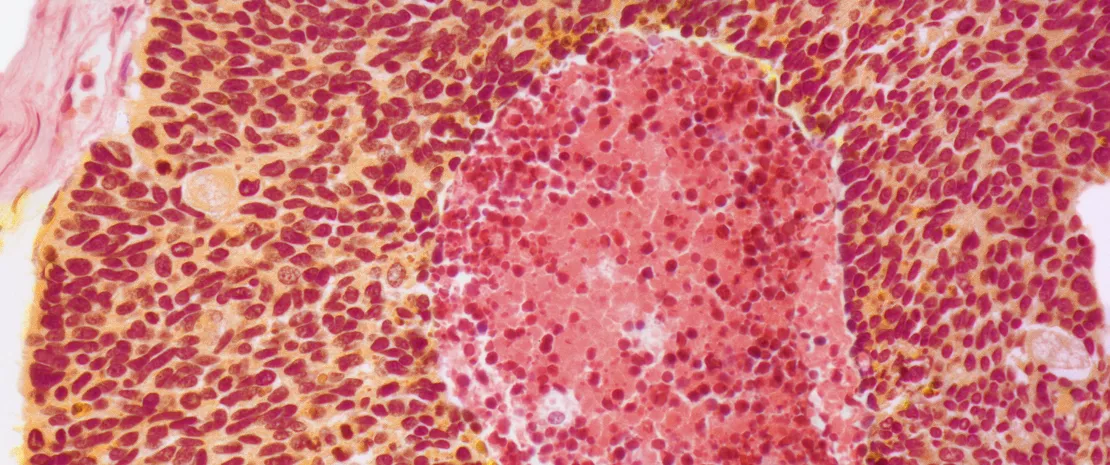
It appears that metabolic and immune interactions between the host and the gut microbiota allow CD8⁺ T cell activation. Various strains of Christensenella minuta appear to selectively boost the efficacy of ILDR and anti-PD-L1 by allowing migration of intestinal PD-L1-expressing dendritic cells to tumor-draining lymph nodes.
According to the authors, a pre-treatment analysis of the gut microbiota could help select patients likely to benefit from this combination therapy, as well as those with dysbiosis who may benefit from fecal microbiota transplantation beforehand.










