Bacterial diarrhea: gut microbiota, a potential victim or a guard against it?
Pathogenic bacteria such as Shigella, Vibrio cholerae, Salmonella, E. coli… lead to bacterial diarrhea, through mechanisms that depend on the bacteria involved. Bacterial diarrheas are accompanied by intestinal dysbiosis. Symmetrically, the gut microbiota exerts effects on the bacterial infection. Since a ‘healthy’ gut microbiota is more resistant to infection, probiotics could reduce the severity of many bacterial infections.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections
About this article
Underlying how lethal bacterial diarrhea can be, these 8 bacteria were responsible for more than a third of the over 1.65 million deaths from infectious diarrhea recorded worldwide in 2016.2
These 8 bacteria
- Shigella: 212,438 deaths.
- Vibrio cholerae: 107,290 deaths.
- Non-typhoidal Salmonella spp: 84,799 deaths.
- Campylobacter spp: 75,135 deaths.
- Enterotoxigenic E. coli: 51,186 deaths.
- Clostridioides difficile: 22,417 deaths.
- Aeromonas: 16,881 deaths.
- Enteropathogenic Escherichia coli: 12,337 deaths.
FROM INFECTION TO DIARRHEA
The mechanisms that lead to bacterial diarrhea depend on the bacteria involved. Transmitted via contaminated food, water or by personto-person contact, Shigella infests the gastrointestinal tract, produces an enterotoxin and serotype toxin 1, destroying the intestinal epithelium and leading to severe bloody and mucous diarrhea.3,5
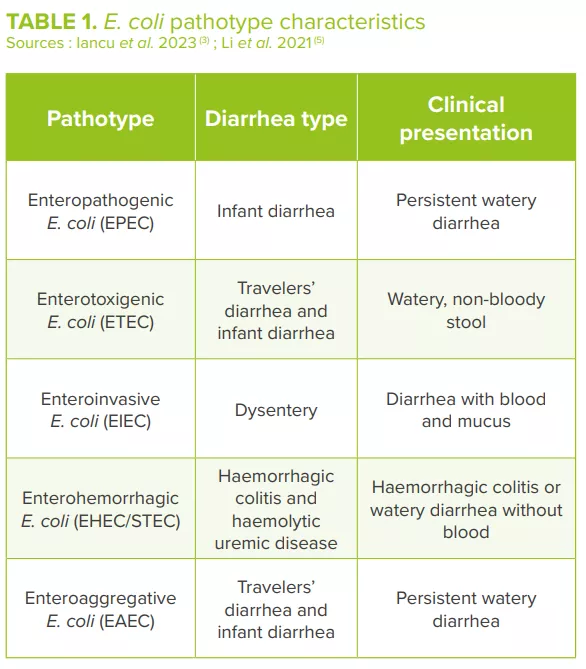
Pathogenic variants of Vibrio cholerae produce a cholera toxin that activates anion secretion, inhibits absorption of electroneutral NaCl and destroys the intestinal barrier function, thereby inducing massive fluid secretion in the lumen of the small intestine and the loss of large amounts of water, sodium, chloride, bicarbonate and potassium.3,5,13 Different pathogenic E. coli strains, classified into different pathotypes (Table 1), cause mild to severe diarrhea usually accompanied by fever. E. coli adheres to the intestinal epithelial cells through the adherent fimbriae, produces toxins and exerts its pathogenic effects.3,5
EFFECT OF PATHOGENS AND DIARRHEA ON MICROBIOTA
Bacterial diarrheas are accompanied by dysbiosis, usually with an overabundance of facultative anaerobes (Escherichia, Streptococcus, Enterococcus, etc.) in dysenteric diarrhea, and a depletion in bacteria of known immuno-modulatory effects (Lactobacillus ruminis, Bifidobacterium pseudocatenulatum)7 (Figure 3).
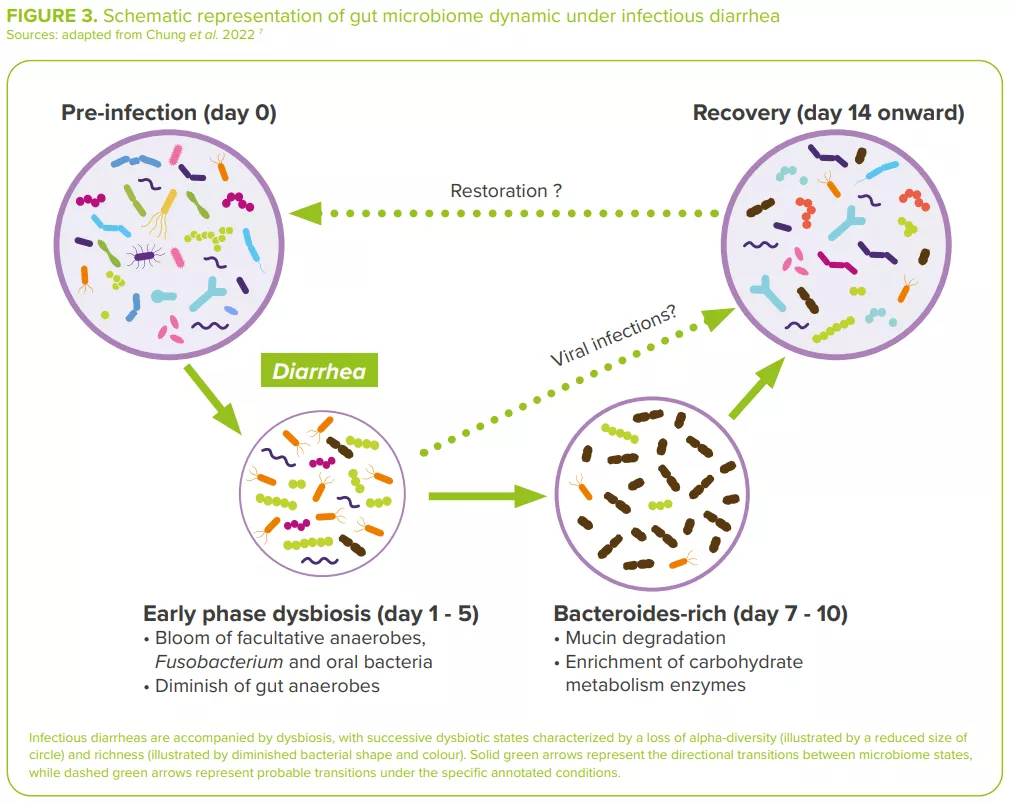
For example, in cholera, the gut microbiota is substantially modified both during and after infection, this as a consequence of the removal of the mucus layer along with the residing gut microbial community and of the delivery of toxin by V. cholerae. 13 During recovery, the gut microbiota of cholera patients slowly repopulates via an accumulation pattern similar to that of the maturation of the gut microbiota observed in children.3
In the same way, children infected with diarrheagenic E. coli (DEC) display a distinctive gut microbial composition, with a high fraction of Bacteroidetes and Proteobacteria and a reduced abundance of Firmicutes. 13 Increases in Proteobacteria could be partially explained by an increase in Escherichia/ Shigella species (as the cause of diarrhea) and in other members of Enterobacteriaceae, such as Citrobacter and Enterobacter (related to histamine production induced by proinflammatory environments and associated with E. coli adherence).14 Frequent antimicrobial use can also partly explain the observed dysbiosis.7
GUT MICROBIOTA PROTECTION AGAINST INFECTIONS
Symmetrically, the gut microbiota has demonstrated effects on bacterial infection. In germ-free animals, their lack of a gut microbiota and the absence of ecological competition results in an immature immune system that renders them highly susceptible to diarrheal pathogens: 10 colony-forming units (CFU) of Salmonella are enough to cause a lethal infection, whereas to kill 50% of mice with an intact gut microbiota 103 –109 CFU are required.8
In humans, Prevotella, Bifidobacterium and Blautia have been shown to reduce colonization of V. cholerae. Conversely, Paracoccus is believed to support the growth of the pathogen.13 This is the reason why promoting a ‘healthy’ gut microbiome has been considered a useful approach in the intervention and prevention of cholera.13
“The GI tract encompasses ~1 to 10 times more bacterial cells than the number of cells in the human body.” 16
BACTERIAL AND YEAST PROBIOTICS, PREBIOTICS AND FMT
The severity of several bacterial infections could be reduced by probiotics: for example, probiotic E. coli inhibits the biofilm formation of other E. coli strains and likewise those of the pathogenic Staphylococcus aureus and S. epidermidis. 3 Regarding dysentery, a combination of Lactobacillus and Bifidobacterium strains and a Streptococcus strain reduces both the duration of blood-affected diarrhea and the time spent in hospital.3
Numerous mechanisms could explain why probiotics alleviate diarrhea:3 production of antimicrobial substances, competitive exclusion, competition with cell binding sites, production of acids and metabolites that lower the surrounding pH, strengthening of the gut mucosal barrier, modulation of gut mucosal immunity and gut microbiota diversity. For example, the probiotic yeast Saccharomyces boulardii may facilitate gut microbiota restoration in children with acute diarrhea.15
Prebiotics can also have a positive impact on diarrhea: by increasing the bacterial production of short-chain fatty acids (SCFAs) such as butyrate, which contribute to the gut barrier integrity; and by antagonizing the adherence of pathogens to epithelial cells, thus inhibiting colonization and promoting gut pathogen elimination.3
Fecal microbiota transplantation (FMT), which aims to restore a healthy gut microbiota, has proven effective and is only indicated in the treatment of recurrent C. difficile in both adults and children.14
CLINICAL CASE by Pr. Aldo Maruy
- A 2-year-old boy presented with fever, abdominal pain and diarrhea with mucus and blood. He had history of two similar episodes in the last six months, treated solely with antibiotics.
- In order to prevent a relapse, it was decided to treat him with antibiotics and probiotics. The diarrhea ceased within 48 hours, the antibiotic was suspended at the 5th day while the probiotic was continued for two weeks; a diet rich in complementary food and prebiotics was prescribed.
- In addition to treating the infection with antibiotics, it is recommended in order to prevent a new diarrheal episode that the composition of the gut microbiota be restored via the diet together with the administration of prebiotics and probiotics

EXPERT OPINION
Throughout one’s life, a healthy microbiota plays an important role in the prevention and treatment of bacterial diarrhea. Specific species have demonstrated protective effects against diarrhea: Lactobacillus taxa are protective against Shigella spp.-induced diarrhea; the presence of Sutterella sp., Prevotella copri and Bacteroides vulgatus predict resistance to enterotoxigenic E. coli (ETEC). On the other hand, microbial intervention, through modifying the diet and using prebiotics, probiotics and FMT, can regulate the composition of gut microbiota to prevent and treat diarrhea. Future research should expand our knowledge of the microbiome as it relates to infectious diarrhea, thereby assisting in the design of improved preventative and managerial interventions.
CONSEQUENCES OF TRAVELERS’ DIARRHEA
When visiting medium- and high-risk destinations, 10–70% of travelers from low infectious disease-risk countries experience diarrhea. Travelers’ diarrhea is predominately caused by bacteria (≥80%–90% of cases), with intestinal viruses accounting for a minimum of 5%–15% of the cases.52 Infections by protozoal pathogens might account for approximately 10% of diagnoses mostly in those traveling for extended periods.
The microbiota of travelers who experienced diarrhea show greater variation throughout the length of their stay than those of healthy travelers, associated with a lower baseline diversity, which has been linked to an increased susceptibility to infection.51
Moreover, diarrhea reduces the capacity of microbiota restoration (large increase of the rate of divergence from baseline) and leads to the acquisition of multidrugresistant organisms.51 Thus, according to a study including 267 Americans travelling outside the United States, a third returned with diarrhea, 61% with intestinal dysbiosis and 38% with antibiotic-resistant bacteria (most of them an E. coli), contributing to the global spread of antimicrobial resistance.58
E. coli, Dorea fomigenerans, Bacteroïdes vulgarus, B. caocae, Odoribacter splanchnicus…,
Ruminococcus bromii, coprococcus, Clostridioides bartlett


