Alcoholic hepatitis: towards new fungal targets?
An international study has shown that a fungal gut dysbiosis could be involved in the pathophysiology of alcoholic hepatitis. This discovery could lead to new treatments and prognostic tools.
Sources
This article is based on scientific information
About this article
Alcoholic liver disease is associated to a high mortality rate and few therapeutic and prognostic innovations. The role of the gut-liver axis was recently brought to light in alcoholism complications, especially through the translocation of gut bacteria to the liver. Could fungal dysbiosis also play a role?
Proliferation of Candida
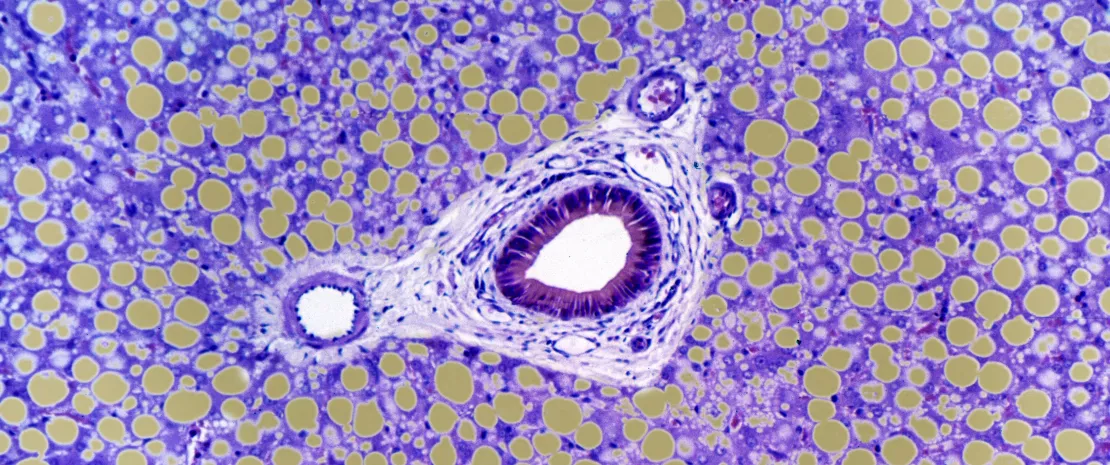
Based on a North American and European cohort, an international team studied the gut mycobiota of 59 patients with alcoholic hepatitis, 15 patients with (sidenote: In the study, problematic alcohol consumption in patients with alcoholic hepatitis was defined as over 50 g/day for men and 40 g/day for women in the last three months; non-problematic drinking is usually defined as under 20 g/day. ) (at different stages of liver damage), as well as 11 control subjects. A clear proliferation of Candida was observed in both groups of patients, as well as lower fungal diversity and abundance compared to the control group where Penicillium was dominant. Besides, a correlation between gut mycobiota and clinical parameters was established: Candida was associated to an increase in pericellular fibrosis, while Penicillium was associated to reduced inflammation and decrease in (sidenote: Mallory bodies Residual clusters of microfilaments secondary to the toxicity of alcohol and its metabolites ) .
Higher immune response
Anti-Saccharomyces cerevisiae antibodies (ASCA) were measured to detect a potential immune response to fungal species, especially to Candida albicans. ASCA levels were significantly higher in the group of patients with alcoholic hepatitis compared to the two other groups: the authors believed that this could be explained by a combination of increased Candida levels and altered fungal phagocytosis. This combination leads to a higher immune response, contrary to subjects with alcohol abuse in whom phagocytosis is maintained. Moreover, ASCA levels and mortality rate were related: starting at 34 IU/ml, mortality at 90 and 180 days was significantly higher, regardless of other confounding factors such as corticosteroid or pentoxyfillin use (reference treatment), (sidenote: MELD score Model for end stage liver disease: reference prognostic score based on the INR (an index representative of prothrombin time), serum bilirubin and serum creatinine ) , or bacterial translocation rate.
New therapeutic options on the horizon
Other studies have shown that cirrhotic patients are exposed to an increased risk of developing fungal infections. Aspergillosis was a frequent and often mortal complication in patients with alcoholic hepatitis. According to the authors, the gut mycobiota is a potential therapeutic target that should be explored. The same applies to ASCA levels combined with the MELD score, which could improve diagnostic with regard to the mortality risk. Before that, these results need to be confirmed since the number of participants in this study was relatively low, and the use of antibiotics by some of them could have influenced the composition of their gut mycobiota.










