How menopause impacts microbiota
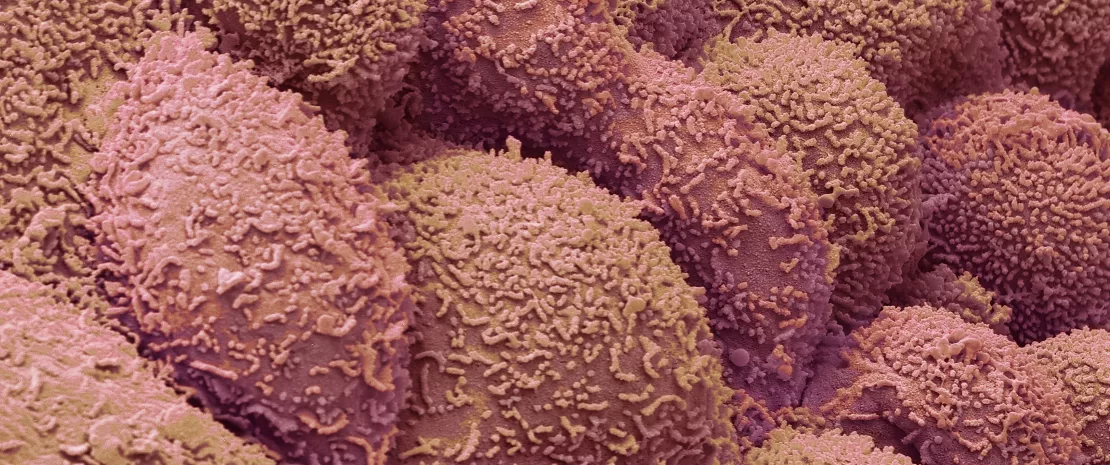
The oral, vaginal, and gut microbiomes undergo significant changes during menopause. A new study suggests this may have consequences for women’s health.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
A narrative review by Spanish researchers has found that the drop in estrogen associated with the menopause significantly disrupts microbiota, with significant repercussions on women’s health. 1 In particular, it leads to significant changes in the oral epithelium (thinning, drying out, etc.), which can affect oral health and the microbial ecosystem living on the mouth’s surface.
This alteration of the oral microbiome is frequently accompanied by a variety of oral symptoms in post-menopausal women.
Oral cavity sees significant change
Saliva becomes less abundant and more acidic, which not only increases the risk of caries and periodontal disease but also disrupts the oral microbiota. (sidenote: Dysbiosis Generally defined as an alteration in the composition and function of the microbiota caused by a combination of environmental and individual-specific factors. Levy M, Kolodziejczyk AA, Thaiss CA, et al. Dysbiosis and the immune system. Nat Rev Immunol. 2017;17(4):219-232. ) of the oral microbiota has also been observed, which is likely to promote colonization by pathogenic bacteria and the onset of mucosal lesions such as angular cheilitis, an inflammation of the corners of the mouth.
Since the cells of the salivary glands and gums carry estrogen receptors involved in immunity, fluctuating hormone levels can cause inflammation of the mucous membranes. This can affect the balance of microorganisms and promote diseases such as candidiasis, which is linked to the proliferation of Candida albicans, or gingivostomatitis, the simultaneous inflammation of the gums and oral mucosa.
Taking these changes in the flora into account could enrich oral health prevention strategies for older women.
Cortisol also affects oral bacteria
Salivary cortisol is a stress marker that is higher in post-menopausal women suffering from psychosomatic disorders of the head and neck (aphthous stomatitis, atypical facial pain, lichen planus, burning mouth syndrome, dry mouth). It may directly alter oral bacterial activity and increase the risk of periodontal disease. For example, one study showed that in the presence of cortisol, certain bacteria were more active, such as Leptotrichia goodfellowii (associated with gingivitis) or members of the Fusobacteria phylum. The study highlights that this hormonal regulation of the microbiome may also extend to the gut-brain axis. These gut disturbances may play a role in age-related inflammatory or neurodigestive disorders.
Greater bacterial diversity in the vaginal microbiota
In the vagina, the menopause is accompanied by a decrease in the dominance of lactobacilli, which normally acidify the vagina, thereby preventing the proliferation of pathogens or an increase in bacterial diversity. This is the famous “ (sidenote: Menopause paradox The menopause paradox, characterized by a decrease in microbial dominance but an increase in richness observed in the vaginal niche, may apply to other body sites within the microbiome community. ) .”
These changes increase susceptibility to bacterial vaginosis and may contribute to diseases such as endometrial cancer. Post-menopausal women with severe symptoms of vaginal dryness, (sidenote: Dyspareunia Recurrent or persistent genital pain during sexual intercourse. ) (pain during intercourse), and vaginal pain, often present greater bacterial diversity than women who do not suffer from these symptoms.
Estrogen and microbiota: a dynamic two-way relationship
Certain bacteria in the microbiota are thought to be able to “deconjugate” estrogen bound to proteins in the blood, thereby rendering these hormones biologically active. They are known as the “estrobolome.” The estrobolome can modify the availability of estrogen and thus influence the physiological processes associated with it. But that’s not all...
Menopausal shift
Menopausal shift includes physiological and histological changes in the host, leading to alterations in the composition and metabolism of the resident microbial community, due to hormonal changes during the aging of women.
While certain bacteria in the gingival and gut microbiota can modulate the effect of estrogens by breaking them down, hormones can in turn directly modulate the activity of bacteria: bacteriostatic or bactericidal effects, stimulation of growth or proteolytic activity, modulation of biofilm formation, etc.
They also pave the way for targeted interventions, such as the use of probiotics to restore protective flora.
All of these bidirectional dynamics between sex hormones and bacteria can be completely disrupted during the menopause, with significant repercussions on women’s health.
These interactions underline the importance of a systemic approach to understanding microbiota.
Towards better care for post-menopausal women
According to the researchers, there are still many unknowns about the interactions between sex hormones and the oral, gut, and urogenital microbiomes. However, with advances in science, new studies should soon give rise to previously unexplored therapeutic avenues (dietary changes, probiotics, personalized interventions, etc.).
The ultimate aim is to alleviate the symptoms of menopause and improve women’s overall health. Stay tuned!













