Factors influencing microbiota development and maturation of the immune system early in life
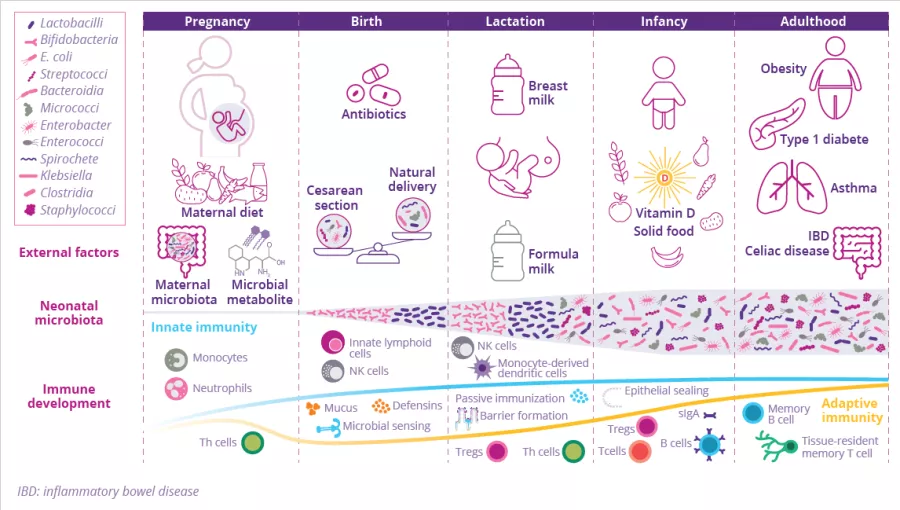
Birth represents the biggest substantial environmental change in life as the newborn is exposed for the first time to a countless variety of microbes which colonize all body surfaces, leading to the establishment of the commensal microbiota in parallel with the immune system. Many factors shape the composition of the gut microbiota and the maturation of the newborn immune system (Fig 3). Discrepancies in the microbiota and immunity crosstalk during each developmental stage can have long-term effects on disease susceptibility.13
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections

About this article
Authors
Birth impacts gut microbiota composition...
by Dr. Travis J. De Wolfe
The mode of delivery impacts what type of bacteria from the mother are transmitted to the neonatal intestine.14 Babies delivered via the birth canal often carry many gut bacteria that synthesize lipopolysaccharide (LPS), a major membrane component of Gram-negative bacteria that can properly train the human immune system to properly respond to microbial threats.15 In contrast, children delivered by caesarean section are predisposed to being colonized by opportunistic pathogens that circulate in hospitals.14
…As well as maturation of immune structure
These differences in initial microbial colonization can affect the subsequent maturation of the local innate lymphoid structures and alter the population of protective regulatory T cells (Treg), resulting in long-term effects on human intestinal physiology. Maturation of T cells and induction of immune factors can protect against, or in some cases, contribute to autoimmune-mediated diseases (diabetes, multiple sclerosis…) that develop later in life.15,16
Antibiotics impact on immune responses
By Dr. Pascal Lavoie
Antibiotics are essential to treat serious bacterial infections, however unnecessary antibiotic exposure can have serious adverse health consequences and should be avoided (ie. when the infection is due to a virus). In older adults, prolonged antibiotic use can lead to the overgrowth of a gut bacterial pathogen called Clostridioides difficile, with potentially life-threatening health consequences, particularly in the elderly.17 Overusing antibiotics can also promote antimicrobial resistance, which can limit treatment options for future infections.18 In animal models, antibiotic based perturbation of the gut microbiome alters immune functions and immune response thresholds.19 Data in humans suggest that unnecessary antibiotic use may increase the risk of developing chronic health problems, like type I diabetes, asthma, allergies or even obesity.20 Prolonged antibiotic use (> 1 week) is known to reduce the diversity of the gut microbiome, with babies born prematurely being the most vulnerable to perturbations in their gut microbiome. Prolonged, broad spectrum antibiotic use in the mother or premature infant reduces gut bacterial diversity, increasing the risk of sepsis and necrotizing enterocolitis.21 Overall, the data in humans support the concept that the gut microbiome plays a major role helping babies develop into healthy adults. While the risks of excessive antibiotic exposure in adults are less severe, they may still impact the development of their immune responses, therefore antibiotic usage at any age should be restricted to those cases where they are necessary.
Dysbiosis is not universal and is defined for each individual, according to their state of health. A common definition describes it as a compositional and functional alteration in the microbiota that is driven by a set of environmental and host-related factors that perturb the microbial ecosystem.9
FIGURE 3: Environmental factors influencing the development of the newborn microbiota and mucosal immune system.
Adapted from Kalbermatter C et al, 202113
Throughout pregnancy, microbial metabolites (originating from the maternal microbiota and diet) influence fetal immune development. At birth, microbiota colonization starts in parallel with development of the immune system. At this stage, the newborn is still dependent on maternal protection, which is ensured through breastfeeding: maternal milk contains mother-derived bacterial antigens that stimulate the maturation of the innate mucosal immune system. Regarding gut microbiota colonization, Enterococcacae, Clostridiaceae, Lactobacillaceae, Bifidobacteriaceae, Streptococcaceae dominate in the first weeks of life. The introduction of solid food in an infant’s diet leads to an increase in gut microbiota diversity, evolving to a more adult-like microbiota: the abundance of Bifidobacteriaceae decreases, while Bacteroides, Ruminococcus, and Clostridium become more prevalent. Birth mode, breast milk, solid food, and the intake of antibiotics are factors that shape the early life microbiota and the neonatal immune system.
PROOF OF CONCEPT: gut microbiota colonization is essential for immune system development
by Dr. Travis J. De Wolfe
Studies with germ-free mice have demonstrated the important role that the microbiota plays in preventing a faulty immune system.22 Germfree mice are impaired in the production of CD4-positive T helper immune cells, whereas selectively colonizing these mice with Clostridia, a commensal bacterial group, can induce the production of these cells that subsequently promote antimicrobial defenses in the gut and protect against pathogen infection.23 IgA antibodies are another critical component of the immune system, that are deficient in germ-free mice. These antibodies bind to commensal bacteria and prevent them from escaping the GI tract. Selective colonization of germ-free mice with an Escherichia coli strain, or distinct Bacteroides strains trigger a rapid restoration/normalization of IgA.24,25