SCFAs: new intestinal markers of Parkinson’s disease?
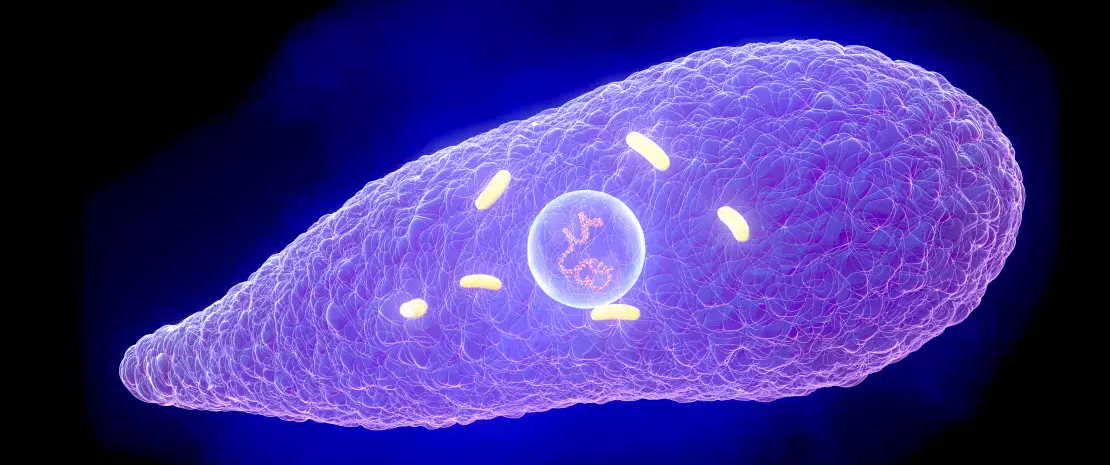
Short-chain fatty acids (SCFAs) are gut microbiota metabolites already known to be involved in Parkinson’s disease, particularly in rodents. But what about in humans?
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
(sidenote: https://parkinsonscare.org.uk/worldparkinsonsday/ ) (April 11) is an opportunity each year for patient associations and health professionals to see how research is progressing on this complex neurodegenerative disease for which there is no treatment to date. This year, discussions will no doubt focus on a new study by a team of Taiwanese researchers. The team wanted to determine whether SCFAs could discriminate between Parkinson’s patients and healthy individuals, and whether there was a correlation with disease severity. To do this, they analyzed plasma and fecal levels of several subtypes of SCFAs in addition to the gut microbiota of 181 participants (96 patients and 85 controls). They also studied the motor and cognitive effects of the disease. The study results were published in Neurology in early 2022.
Different fecal and plasma SCFA levels in Parkinson’s patients
In Parkinson’s patients, the results showed reduced fecal SCFA levels compared to healthy individuals (butyric acid, valeric acid and propionic acid), whereas plasma levels were higher.
Another takeaway: fecal quantities of the same SCFAs were lower in patients with advanced Parkinson’s disease compared to patients in the early stages of the disease.
Correlation between SCFA levels and symptom severity
Fecal and plasma concentrations vary depending on the severity of motor and cognitive symptoms.
More severe motor impairment is correlated with a low fecal concentration of most SCFAs, coupled with an increased plasma propionic acid concentration.
More serious cognitive symptoms are associated with lower fecal levels of butyric acid and higher plasma concentrations of butyric acid and valeric acid.
Link between the composition of patient microbiota and SCFAs
The study showed that microbial diversity in Parkinson’s patients differed from that in healthy patients. This study highlights the correlation between SCFA concentrations and the abundance of pro-inflammatory bacteria (Clostridiales and Ruminococcus), particularly in the case of propionic acid. This supports the hypothesis that gut inflammation is associated positively with disease aggravation.
Specifically, these results suggest that SCFAs may serve as gut biomarkers for Parkinson’s disease and also reflect severity. This is an interesting scientific advance, which may pave the way for more accurate diagnosis and better patient management.







