What is the impact of Covid-19 on the human microbiome?
Overview
By Pr. Gerard D. Wright
M.G. DeGroote Institute for Infectious Disease Research, McMaster University, Hamilton, Canada
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
Sections

About this article
Author
The COVID-19 pandemic is impacting human health in profound ways. Finlay et al. explore how COVID-19 and our response to it are affecting the human microbiome and what the results of the pandemic may be on maintaining our health beyond acute viral infection [1]. Both SARS-CoV-2-infected and uninfected persons have the potential to have their microbiomes significantly altered by the pandemic with ensuing effects on health. There is growing evidence that the diversity of the human microbiome is decreasing in individuals across the globe, with an acceleration over the past several decades and concomitant increase in chronic non-communicable diseases. The COVID-19 pandemic can exacerbate these concerns of diminished microbial diversity through several mechanisms (increased hygienic procedures, changes in food access, general decrease in social and community interactions…). What is less evident at this stage is what the long-term effects of the pandemic will be on the microbiome and, as a result, human health. The current situation of COVID-19 offers a unique “living laboratory” opportunity to study in real-time how pandemics can impact human health in the shortand long-term and across the lifespan and what these effects might have on individuals, communities, and societies.
What is already known about this subject?
The diversity of the human microbiome varies across the globe. It is impacted by nutrition, geography, income and wealth, and societal structures [2]. A general trend of loss of microbiome diversity, especially in wealthy countries, is correlated with changes in diet (increased consumption of processed food), access to clean water, antibiotics use (and abuse), and general improvement in hygiene. The original “hygiene hypothesis” and its more recent elaborations suggest that this reduction in microbial diversity is directly linked to insufficiently “trained” immune responses, especially in the early stages of life that are manifested in susceptibility to a range of downstream chronic conditions (obesity, asthma, cardiovascular disease) [3]. Such conditions are also known to increase susceptibility to infections. Similarly, aging is often associated with a shift towards diminished genetic diversity of the human microbiota and increased susceptibility to infection [4]. From the past year’s experience, we know that individuals with underlying chronic conditions and the elderly – and thus are predicted to harbor a less diverse microbiome – have been disproportionally affected by SARS-CoV-2 infection with adverse outcomes. This observation may not be coincidental. Moreover, SARS-CoV-2 infection is frequently associated with gastrointestinal disorders [5] correlated with the presence of ACE-2 receptors [6], and associated with gut dysbiosis.
What are the main results of this study?
The near-universal increased use of hand sanitizers, deep cleaning of buildings and public places, and even the wholesale application of anti-infective agents in open outdoor spaces have unknown effects on microbial diversity. Changes in food access and intake are also predicted due to increased home cooking, alcohol consumption, and potential food security concerns for some parts of the world due to reduced travel and access to goods. Altered social patterns may also have profound impacts on microbiome diversity. Lockdowns, lack of human contact in the workplace, cloistering of long-term care facilities have the potential to modulate human microbiomes in ways that increase inflammation and risk of infection. It is also important to recognize that there remain hygiene inequalities across the globe, and by implication different impacts on human microbiomes. These are playing out in different relationships with COVID-19 disease, for example water quality scores were inversely correlated with COVID-19-related deaths in one study [7]. All these areas require significant study and attention.
What are the practical consequences?
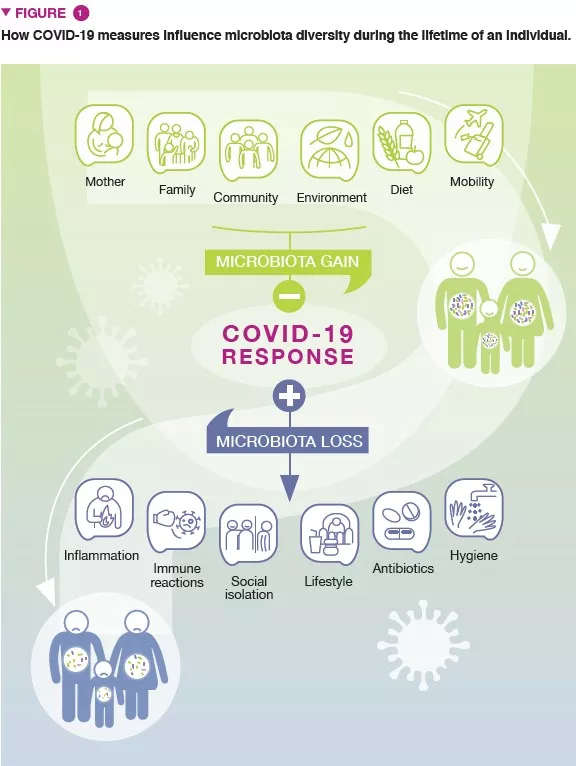
Finlay et al. argue that the effects of the COVID-19 pandemic on microbiome diversity and health should be investigated in real-time and over the long term across the lifespan (Figure 1). It offers the opportunity to look back to the impacts of past infectious disease events with more clarity and to guide response and resilience in future pandemics. Longitudinal studies can also be marshaled to address future challenges armed with information on how the microbiota can impact human health beyond acute infection. Already reports are emerging on pandemic-related changes to the human microbiome, including how travel patterns are influencing microbiome diversity [8] that even after six months post-disease that SARS-CoV-2-infected patients do not have fully recovered microbiome diversity [9]. Altered practices in neonatal care, at least in the early stages of the pandemic, such as limited skin-to-skin contact and reduced breastfeeding, have the potential to alter the infant microbiota, with potential health effects over the longterm. On the other hand, increased contact with household pets and children in cases where parents can work from home may have a balancing effect. Finally, the effect on younger children and adolescents who often have not had an opportunity to attend school or engage in sporting and social events have diminished normal contact with others is unknown. The influences that sustained stress induced by isolation, decreased social engagement, etc., may have on the long-term health of individuals due to microbial changes will need to be measured for years to come.
Conclusion
The diversity of the microbiome is essential to human health, and there is a correlation between diminished microbial diversity with increased risk to develop chronic diseases and susceptibility to infections. The intersection of the COVID-19 pandemic and microbiome health exposes vulnerabilities to this line of defense to acute infection and long-term health. While the pandemic is global, it is being felt unequally across nations and communities. How the inequities in age, health, nutrition, hygiene access and societies manifest themselves in short and long-term health impact related to microbiome disruption is unknown at present, but they must be recognized and studied.
1 Finlay BB, Amato KR, Azad M, et al. The hygiene hypothesis, the COVID pandemic, and consequences for the human microbiome. Proc Natl Acad Sci USA 2021; 118: e2010217118.
2 Porras AM, Brito IL. The internationalization of human microbiome research. Curr Opin Microbiol 2019; 50: 50-5.
3 Stiemsma LT, Reynolds LA, Turvey SE, et al. The hygiene hypothesis: current perspectives and future therapies. Immunotargets Ther 2015; 4: 143-57.
4 DeJong EN, Surette MG, Bowdish DME. The gut microbiota and unhealthy aging: disentangling cause from consequence. Cell Host Microbe 2020; 28: 180-9.
5 Cha MH, Regueiro M, Sandhu DS. Gastrointestinal and hepatic manifestations of COVID-19: A comprehensive review. World J Gastroenterol 2020; 26: 2323-32.
6 Vuille-Dit-Bille RN, Lischty KW, Verrey F, et al. SARS-CoV-2 receptor ACE2 gene expression in small intestine correlates with age. Amino Acids 2020; 52: 1063-5.
7 Kumar P, Chander B. COVID 19 mortality: Probable role of microbiome to explain disparity. Med Hypotheses 2020; 144: 110209.
8 Peng Y, Zhang D, Chen T, et al. Gut microbiome and resistome changes during the first wave of the COVID-19 pandemic in comparison with pre-pandemic travel-related changes. J Travel Med 2021 [Epub ahead of print].
9 Chen Y, Gu S, Chen Y, et al. Six-month follow-up of gut microbiota richness in patients with COVID-19. Gut 2021 [Epub ahead of print].







