A new lens on chlamydia: beyond behavior, into the microbiome
What if the key to predicting and preventing Chlamydia isn’t behavior, but bacteria? A groundbreaking study 1 reveals a vaginal microbiome signature that doubles infection risk and predicts reinfection, reshaping how we understand sexually transmitted infection (STI) vulnerability.
Lay public section
Find here your dedicated section
Sources
This article is based on scientific information
About this article
Author
For decades, the conversation around Chlamydia trachomatis, the most common bacterial sexually transmitted infection globally, has revolved around sexual behavior: number of partners, condom use, prior STI history.
But a groundbreaking new study published in Cell 1 invites us to reframe that narrative. Instead of focusing solely on behavior, we’re asked to consider a more intimate and microscopic protagonist: the cervicovaginal microbiome (CVM).
128.5 million In 2020, an estimated 128.5 million new cases of Chlamydia were recorded globally among adults aged 15 to 49. ²
In a longitudinal study, researchers tracked 560 Black and Hispanic adolescent and young adult (AYA) women in New York City, communities disproportionately impacted by Chlamydia infections.
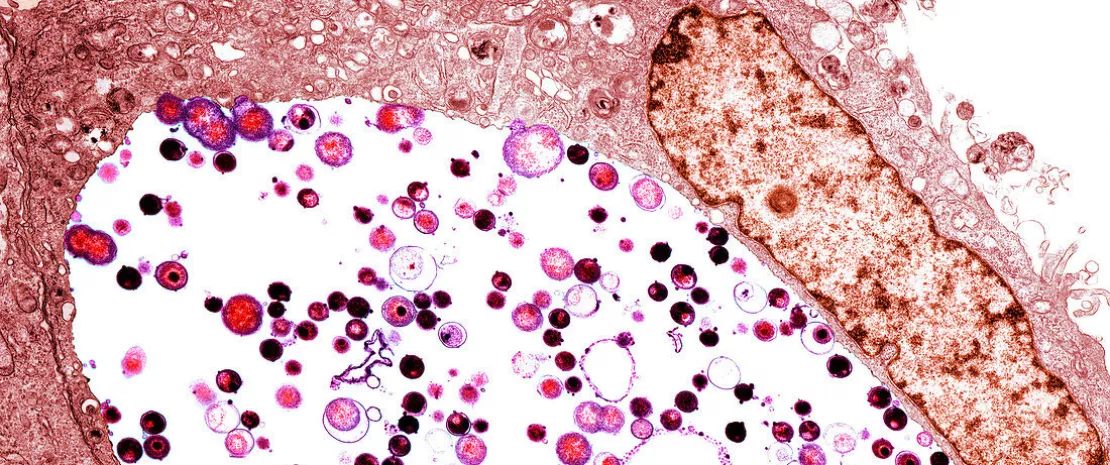
They followed participants before, during, and after an incident Chlamydia infection. But rather than just charting symptoms or behaviors, they analyzed the entire microbial community of the cervicovaginal tract using high-resolution 16S rRNA and ITS1 gene sequencing.
The result? A nuanced and highly predictive microbial fingerprint for Chlamydia risk, reinfection, and even possible complications like pelvic inflammatory disease (PID) and miscarriage.
mBV-A and CST-IV-A: microbial fingerprints of risk
The team used a powerful molecular algorithm (molBV) to quantify bacterial vaginosis (BV)-like states, then categorized microbial communities into “Community State Types” (CSTs).
Among these, CST-IV-A, dominated by Candidatus Lachnocurva vaginae, emerged as the microbial signature most strongly associated with incident Chlamydia infection.
When CST-IV-A overlapped with a high molBV score, a state dubbed mBV-A, the risk of acquiring Chlamydia skyrocketed. Women with this mBV-A profile had more than double the risk of infection compared to those with a Lactobacillus-dominant microbiome (e.g., L. crispatus).
Even more striking? This elevated risk existed months before infection, revealing mBV-A not as a result of Chlamydia, but as a harbinger. This microbial landscape, characterized by high diversity and a drop in protective Lactobacilli, undermines the vaginal environment's natural defenses. It’s not just about pH or lactic acid.
Community State Type (CST)
A classification system used to categorize the vaginal microbiome based on dominant bacterial species. For example, CST-I is typically dominated by Lactobacillus crispatus, while CST-IV includes diverse, non-Lactobacillus species often linked to bacterial vaginosis.
molBV Score (Molecular Bacterial Vaginosis Score)
A computational tool that converts 16S rRNA sequencing data into a Nugent-like score (1–10) to assess bacterial vaginosis status. Higher scores indicate greater dysbiosis, mimicking the diagnostic utility of microscopic BV assessment.
(sidenote:
Candidatus Lachnocurva vaginae
A bacterium commonly found in women with bacterial vaginosis and strongly associated with CST-IV-A. It is not yet cultivable in the lab ("Candidatus" denotes this) but has been implicated in increased susceptibility to sexually transmitted infections like Chlamydia.
)
, the star of CST-IV-A, may metabolize D-lactate, a compound with antimicrobial properties, potentially weakening the cervicovaginal defense against pathogens like Chlamydia.
And it doesn’t stop there. The researchers identified a network of 10 bacterial genera, including Prevotella, Megasphaera, and Clostridium, tightly linked and predictive of infection. These weren’t isolated villains; they were a microbial clique.
Their collective presence formed a (sidenote: Microbial Risk Score (MRS) A composite score representing the cumulative risk posed by a group of specific microbial taxa associated with disease. In this study, it predicts Chlamydia risk based on the presence and abundance of 10 interrelated bacterial genera. ) (MRS), essentially a microbial polygraph test, that outperformed any single genus in predicting Chlamydia acquisition.
Reinfection, recovery, and the microbial set point
Even after treatment, the microbiome tells a story. Most women treated for Chlamydia saw their microbiome shift back toward its pre-infection state. But among those who carried the mBV-A profile post-treatment, the risk of reinfection tripled.
One in five previously infected women experienced reinfection, compared to just 4% of controls. The CVM, in a sense, carried a microbial “memory” of susceptibility, one that wasn't erased by antibiotics.
This points to a deeper truth: treatment of the pathogen does not equal treatment of the terrain. Even more provocatively, the researchers found that some women developed the high-risk mBV-A profile after antibiotic treatment, raising questions about how treatment regimens may unintentionally reshape the microbiome in ways that increase future vulnerability.
There were also early signs, though limited by small sample size, that this microbial fingerprint may be associated with complications like PID and miscarriage.
What this means for clinical practice
Traditionally, we’ve focused on patient behaviors: partner count, condom use, STI history. These remain important. But now, clinicians may need to consider a biological susceptibility, encoded not in DNA, but in a dynamic microbial ecosystem.
This research doesn’t just challenge the dogma; it builds a roadmap for integrating microbial diagnostics into sexual health. The cervicovaginal microbiome isn’t just a passive passenger. It’s driving women’s care. And it’s time we pay attention to the route it’s taking.














