The urinary microbiota
The urinary microbiota: what is it and why is it so important for our health?
The human urinary tract is inhabited by numerous microorganisms that can play a protective role in our health.1 Reduced diversity in the urinary flora may also be a risk factor for disease.2 In fact, urine was once thought to be sterile, but recent scientific research has shown the opposite to be the case.2 Continue reading to see how research on the urinary microbiota is evolving.
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information
Sections

About this article
Table of contents
Table of contents
What is exactly the human urinary microbiota?
You have probably heard less about the urinary microbiota than its more well-known neighbors, the gut microbiota and the vaginal microbiota. This is no surprise, since it is a less rich and diverse environment3 whose role requires further research.1
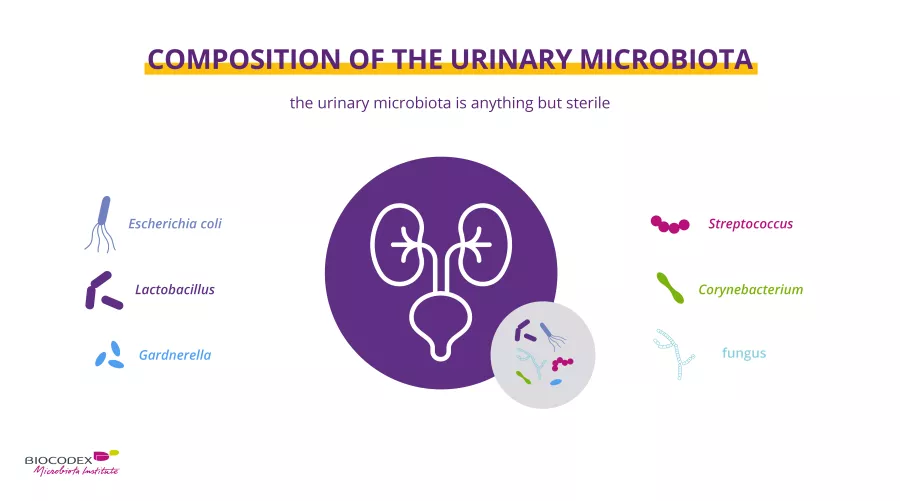
However, recent studies have shown that the urinary tract is home to a unique urinary microbiota.4,5 Urine analyses based on culture-dependent methods have traditionally identified (sidenote: Pathogens A pathogen is a microorganism that causes, or may cause, disease. Pirofski LA, Casadevall A. Q and A: What is a pathogen? A question that begs the point. BMC Biol. 2012 Jan 31;10:6. ) responsible for urinary tract infections (UTIs), such as Escherichia coli.
Advances in detection technologies have led to the discovery of additional bacteria in the urinary microbiota. The genus Lactobacillus is frequently identified, while Gardnerella, Streptococcus, and Corynebacterium also tend to be present, although to a lesser degree.3 In addition, communities of fungi have also been observed.6
Moreover, although the number of studies in the area remains limited, the composition of the urinary microbiota of women appears to be different from that of men,7 which is not surprising given the anatomical and hormonal differences between the two sexes.
Why is the urinary microbiota a key player in our health?
(sidenote: Microorganisms Living organisms that are too small to be seen with the naked eye. They include bacteria, viruses, fungi, archaea and protozoa, and are commonly referred to as “microbes”. What is microbiology? Microbiology Society. ) inhabiting the urinary microbiota can play a protective role in our health.1 However, under certain conditions, they can also influence urinary tract infections.2
Several mechanisms have been described: for example, the bacterial genera Lactobacillus and Streptococcus secrete lactic acid, which is believed to play a protective role against pathogens.8 Lactic acid lowers the pH of urine (≈ 4.5), creating a microenvironment that is hostile to most pathogenic bacteria.
Furthermore, (sidenote: Lactobacilli Rod-shaped bacteria whose main characteristic is the production of lactic acid, from where they get the name “lactic acid bacteria”. Lactobacilli are present in the oral, vaginal and gut microbiota of humans, but also in plants and animals. They are found in fermented foods, such as dairy products (e.g. certain cheeses and yoghurts), pickles, sauerkraut, etc. Lactobacilli are also found in probiotics, with certain species recognized for their beneficial properties. W. H. Holzapfel et B. J. Wood, The Genera of Lactic Acid Bacteria, 2, Springer-Verlag, 1st ed. 1995 (2012), 411 p. « The genus Lactobacillus par W. P. Hammes, R. F. Vogel Tannock GW. A special fondness for lactobacilli. Appl Environ Microbiol. 2004 Jun;70(6):3189-94. Smith TJ, Rigassio-Radler D, Denmark R, et al. Effect of Lactobacillus rhamnosus LGG® and Bifidobacterium animalis ssp. lactis BB-12® on health-related quality of life in college students affected by upper respiratory infections. Br J Nutr. 2013 Jun;109(11):1999-2007. ) produces additional substances, antibacterial metabolites such as hydrogen peroxide, which also protect against pathogens.9 As with the gut microbiota, the urinary microbiota acts as a barrier against pathogens.1
What diseases are associated with an unbalanced urinary microbiota?
As with all microbiota (gut microbiota, lung microbiota, etc.), when the composition of the urinary microbiota is disrupted, an imbalance, or “ (sidenote: Dysbiosis Generally defined as an alteration in the composition and function of the microbiota caused by a combination of environmental and individual-specific factors. Levy M, Kolodziejczyk AA, Thaiss CA, et al. Dysbiosis and the immune system. Nat Rev Immunol. 2017;17(4):219-232. ) ”,9 results. Studies comparing the urinary microbiota of healthy subjects to that of patients suffering from various urinary diseases have identified a link between these diseases and the composition of the urinary microbiota.
In fact, studies published to date have demonstrated a clear role for the urinary microbiota in urinary tract infections (UTIs).8,10 For example, decreased diversity in the urinary microbiota may be a risk factor for urinary tract infections.11
Furthermore, disorders such as urgency urinary incontinence,12 interstitial cystitis,13 and sexually transmitted infections14 have also been associated with an altered urinary microbiota.
How can we take care of our microbiota? We can have a direct influence on it.
-
Diet: it is common knowledge that dietary factors can influence the risk of urinary tract infections. Certain food and dietary products (such as cranberry juice or fermented dairy products containing probiotics) may help reduce the risk of recurrent infection by regulating the microbiota.8
-
Probiotics: oral and vaginal probiotic have been successful in decreasing recurrence rates for UTIs.15
-
Water: drinking plenty of water is important, but researchers have not yet confirmed that it can cure UTIs.1
All the information in this article comes from scientific approved sources. Keep in mind this is not exhaustive. Here are all the studies from which we took all of that information.