Infantile colic
“My newborn baby’s cry is the most heartbreaking sound I’ve ever heard”.1 So confess many parents who turn up helpless at their pediatrician’s office, unable to soothe their baby’s inexplicable cries. The symptoms are often difficult to identify and can be an ordeal for parents, and so it’s important to know how to recognize and understand them. Does the answer lie in your baby’s gut microbiota?
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information
Sections

About this article
What is infantile colic?
Infantile colic is characterized by excessive crying for unknown reasons in otherwise healthy infants. Gastrointestinal disorders (e.g. immaturity of the gastrointestinal tract, an allergy or intolerance to cow’s milk, stomach reflux)2 are mainly to blame,3 but other causes unrelated to the gastrointestinal system,3 such as parental stress,4 or maternal smoking, have also been studied.2
Colic is common in babies, but its symptoms, such as persistent crying, can cause distress in parents.
Did you know?
The word “colic” comes from the Greek “κoλικóς” (kolikos), in reference to the colon. However, despite years of research, the cause of infantile colic remains unknown and it is not entirely certain that the intestines (and therefore the colon) are involved.5
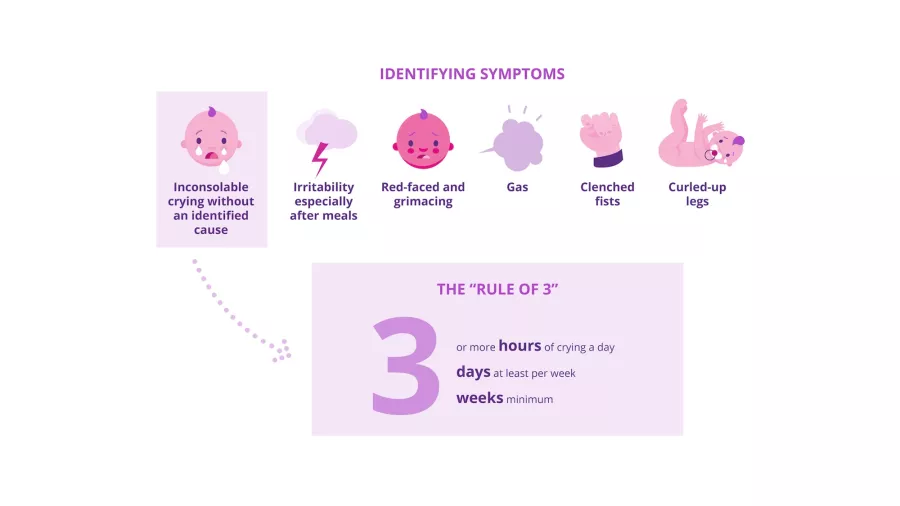
What are the symptoms of infantile colic?
The baby cries a lot, is inconsolable, grimaces and may have a red face. It keeps its fists clenched and may have gas.5 Pediatricians have long used the “rule of three” to diagnose infantile colic.6 Introduced in 1954, these criteria have since been adapted by an international organization to give a new definition with the following criteria: recurrent and prolonged periods of restlessness, crying or irritability without obvious cause such as stunted growth, fever or ill health, and which cannot be prevented or resolved by the caregivers.7
What is the gut microbiota’s role?
A link between infantile colic and the gut microbiota – also known as the gut flora – has recently been established.8 Studies have shown that the gut microbiota of infants affected by colic differs from that of other babies:9
- Their microbiota is less rich in beneficial bacteria, particularly
(sidenote:
Bifidobacterium
A genus of Y-shaped bacteria, most species of which are beneficial to humans. They are found in the gut of humans, and in some yogurts.
They:
- Protect the gut barrier
- Participate in the development of the immune system and help fight inflammation
- Promote digestion and improve symptoms of gastrointestinal disorders Sung V, D'Amico F, Cabana MD, et al. Lactobacillus reuteri to Treat Infant Colic: A Meta-analysis. Pediatrics. 2018 Jan;141(1):e20171811. O'Callaghan A, van Sinderen D. Bifidobacteria and Their Role as Members of the Human Gut Microbiota. Front Microbiol. 2016 Jun 15;7:925. Ruiz L, Delgado S, Ruas-Madiedo P, et al. Bifidobacteria and Their Molecular Communication with the Immune System. Front Microbiol. 2017 Dec 4;8:2345. ) and (sidenote: Lactobacilli Rod-shaped bacteria whose main characteristic is the production of lactic acid, from where they get the name “lactic acid bacteria”. Lactobacilli are present in the oral, vaginal and gut microbiota of humans, but also in plants and animals. They are found in fermented foods, such as dairy products (e.g. certain cheeses and yoghurts), pickles, sauerkraut, etc. Lactobacilli are also found in probiotics, with certain species recognized for their beneficial properties. W. H. Holzapfel et B. J. Wood, The Genera of Lactic Acid Bacteria, 2, Springer-Verlag, 1st ed. 1995 (2012), 411 p. « The genus Lactobacillus par W. P. Hammes, R. F. Vogel Tannock GW. A special fondness for lactobacilli. Appl Environ Microbiol. 2004 Jun;70(6):3189-94. Smith TJ, Rigassio-Radler D, Denmark R, et al. Effect of Lactobacillus rhamnosus LGG® and Bifidobacterium animalis ssp. lactis BB-12® on health-related quality of life in college students affected by upper respiratory infections. Br J Nutr. 2013 Jun;109(11):1999-2007. ) ,8 which can modulate immune responses to protect against colic.5 - Instead, their microbiota appears to be colonized by Escherichia coli,5 Klebsiella or other potentially pathogenic species.5
This gut microbiota imbalance, known as a “
(sidenote:
Dysbiosis
Generally defined as an alteration in the composition and function of the microbiota caused by a combination of environmental and individual-specific factors.
Levy M, Kolodziejczyk AA, Thaiss CA, et al. Dysbiosis and the immune system. Nat Rev Immunol. 2017;17(4):219-232.
)
”, appears to be strongly linked to colic: according to one hypothesis, an altered gut microbiota composition modifies intestinal motility (the way in which food moves through the digestive system), resulting in excessive production of gas.5
Gut inflammation: follow the calprotectin
The protein calprotectin can be used to identify gut inflammation. It is found in large quantities in infants suffering from colic and is associated with reduced gut microbiota diversity.9
How to help babies... and parents?
The family doctor is still the first port of call to diagnose infant colic and reassure parents. There is no cure10 for colic, but a few simple daily practices can help relieve the symptoms. These include breastfeeding, carrying your baby and balancing your child’s gut microbiota, particularly using probiotics.5 Probiotics appear to be a promising avenue, since the intake of “good” bacteria for a few months may reduce gut inflammation6 and help shorten the daily duration of crying.11 Since they help maintain a good intestinal balance, probiotics can also be used as a preventative measure.5
This article is based on scientifically approved sources but is not a substitute for medical advice. If your child displays symptoms, please consult your family doctor or pediatrician.
1 Groopman J. The Colic Conundrum. The crying that doctors can’t stop. Annals of Medicine, Sept 17, 2007 Issue. https://www.newyorker.com/magazine/2007/09/17/the-colic-conundrum
3 Gupta SK. Is colic a gastrointestinal disorder? Curr Opin Pediatr. 2002 Oct;14(5):588-92.
8 Verduci E, Arrizza C, Riva E, et al. Microbiota and infantile colic: what’s new? Int J Probiotics Prebiotics. 2013; 8(1):25–28
15 Tannock GW. A special fondness for lactobacilli. Appl Environ Microbiol. 2004 Jun;70(6):3189-94.
BMI-21.18