Antibiotic resistance: an odd “souvenir” from exotic destinations
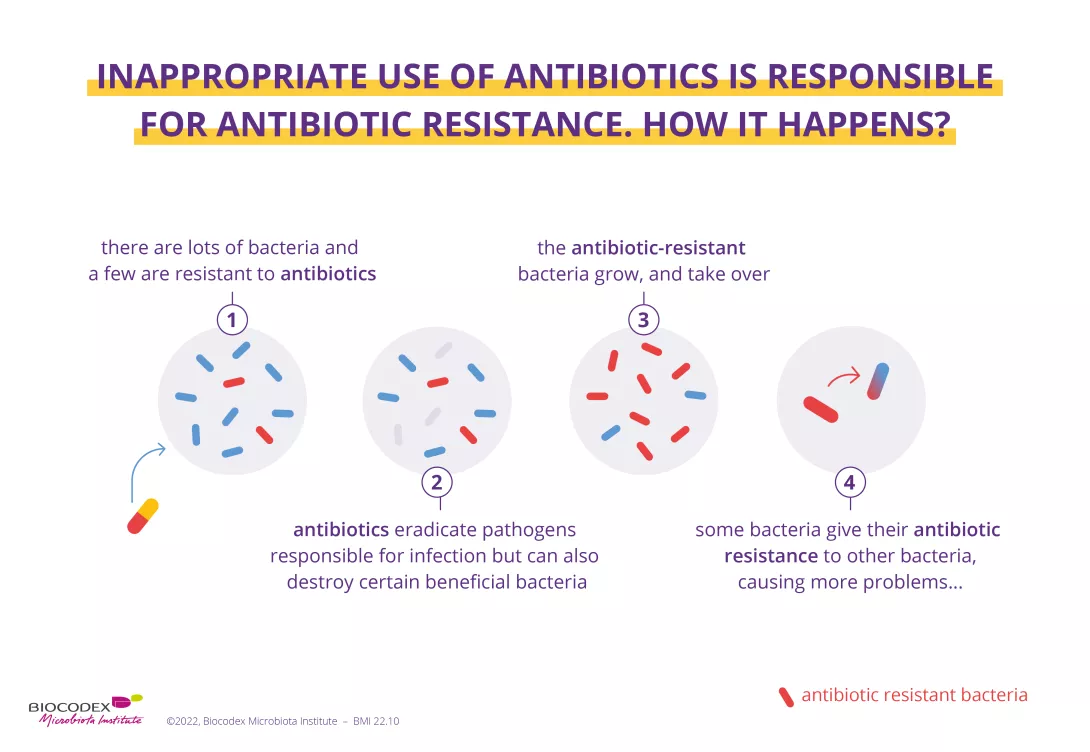
An incredible medical breakthrough becomes the victim of its own success. Since they were first discovered in the early 20th century, antibiotics have saved millions of lives. However, the wide scale and sometimes inappropriate use of these drugs is making them less and less effective at treating infections. The result is that many bacteria have now become resistant! But their excessive and incorrect use cannot take the whole blame for antibiotic resistance.
One study1 has revealed that international travel is increasing the acquisition of antimicrobial resistance genes and could be helping the spread of antibiotic resistance. Head straight to the departure lounge for more information.
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information

About this article
Every year since 2015, the World AMR Awareness Week (WAAW) has been raising awareness of the rise in (sidenote: Antimicrobial Resistance Antimicrobial Resistance occurs when bacteria, viruses, fungi, and parasites change over time and no longer respond to medicines. Antibiotics and other antimicrobial medicines stop working, and infections become harder and even impossible to treat. This resistance to microbes increases the risk of disease spread, severe illness, and death. Antibiotic resistance means the resistance of bacteria to antibiotics. Source: Antimicrobial resistance. October 26, 2020. ) . Linked to the incorrect and overuse of antibiotics, this is when a bacterium is able to resist the action of an antibiotic. In 2020, the WAAW broadened the scope of its message to include (sidenote: Antimicrobials Medicines – including antibiotics, antivirals, antifungals and antiparasitics – used to prevent and treat infections in humans, animals and plants. WHO Antimicrobial Resistance; Nov 2023 ) - antivirals, antifungals and antiparasitics, etc., that is medicines that are essential for fighting (sidenote: Pathogens A pathogen is a microorganism that causes, or may cause, disease. Pirofski LA, Casadevall A. Q and A: What is a pathogen? A question that begs the point. BMC Biol. 2012 Jan 31;10:6. ) (sidenote: Microorganisms Living organisms too small to see with the naked eye. This includes bacteria, viruses, fungi, archaea, protozoa, etc., collectively known as ’microbes’. Source: What is microbiology? Microbiology Society. ) . By reducing our options for treating infections, antibiotic resistance has become a threat to everyone’s health2. Several studies are therefore underway to understand how this phenomenon is spreading so we can better control it, or even stop it altogether.
Antibiotics save life! Did you know that they also have an impact on your microbiota? Did you know that the misuse and overuse of antibiotics can lead to antibiotic resistance? Have you heard about the World AMR Awareness Week
(WAAW)? All the answers in this dedicated page:
Antibiotics: what impact on the microbiota and on our health?
Antibiotic resistance flying beneath the radar
We now know that antibiotic resistance is mainly due to the overuse of antibiotics in human medicine, as well as in livestock and agriculture2. However, a recent study has revealed an unexpected cause of this spread: holidays and business trips to far-flung destinations! In fact, international travel encourages the spread of (sidenote: Gene A gene is the basic physical and functional unit of heredity. Genes are made up of DNA. Source: What is a gene? MedlinePlus.gov. ) in the gut. Researchers studied 190 Dutch travelers, divided into four subgroups based on destination. They were all destined for areas badly affected by antibiotic resistance, namely South East Asia, South Asia, North Africa, and East Africa The aim was to determine whether international travel to these regions could encourage the spread of resistance to areas less badly affected. In order to measure the abundance of these genes in the gut, a stool sample was taken from each participant before and after travel.
A diplomatic bag for antibiotic resistance in the gut?
Using cutting edge technology (
(sidenote:
Metagenomics
A method of studying the genetic material in samples taken directly from complex natural environments (intestines, oceans, soil, air, etc.), as opposed to samples grown in a laboratory. It produces a description of the genes contained in the sample, as well as an insight into the functional potential of the microbial community.
Source: Riesenfeld CS, Schloss PD, Handelsman J. Metagenomics: genomic analysis of microbial communities. Annu Rev Genet. 2004;38:525-52.
)
), the team observed an increase in the number of antibiotic resistance genes between departure and return, especially in travelers coming back from South East Asia. A total of around fifty antibiotic resistance genes was detected following travel. These included genes with well-known and long-standing resistance to antibiotics (such as β-lactams, tetracyclines and fluoroquinolones) as well as new, never-before seen genes.
Could travel pose a danger for public health?
The results of this study are clear: international travelers, colonized by resistance genes whilst on their travels, could unwittingly be bringing back antibiotic-resistant bacteria along with the rest of their luggage. Faced with the risk of this resistance spreading, the authors sound the alarm and highlight the importance of taking rapid action in countries particularly affected by antibiotic resistance. This resonates with the WHO's campaign.
Each year, since 2015, the WHO organizes the World AMR Awareness Week (WAAW), which aims to increase awareness of global antimicrobial resistance.
Antimicrobial resistance occurs when bacteria, viruses, parasites and fungi change over time and no longer respond to medicines. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat, increasing the risk of disease spread, severe illness and death.
Held on 18-24 November, this campaign encourages the general public, healthcare professionals and decision-makers to use antibiotics, antivirals, antifungals and antiparasitics carefully, to prevent the further emergence of antimicrobial resistance.














