Microbiota and exposome: a dialog at the core of our health
Everything we eat, breathe, or apply to our bodies comes into contact with our microbiota, resulting in a non-negligible impact on our health.
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information

About this article
Table of contents
Table of contents
The problem is that many features of the external exposome (low-fiber or high-fat diet, emulsifiers, heavy metals, phthalates, microplastics, fine air particles, pesticides, environmental pollutants, stress, etc.) can upset the balance of our microbiota and lead to dysbiosis.
We know that dysbiosis is linked to numerous chronic diseases, such as obesity, type 2 diabetes, asthma, chronic inflammatory bowel disease, autoimmune diseases, depression, and cerebral development disorders 1.
Collapse of biodiversity = microbiota and health at risk
This ticking time bomb has been confirmed by international expert group IPBES : biodiversity is “declining globally at rates unprecedented in human history” 13 . This collapse is the result of global warming, over-exploitation of land, and pollution.
That’s a problem for our microbiota, since fewer animal and plant species means less microbial diversity in ecosystems and therefore more alteration of microbiota-mediated immunomodulatory circuits, as well as more allergies and autoimmune diseases 14.
Microbiota: a well-connected network that influences health
According to the World Allergy Organization, the loss of biodiversity results in reduced interaction between environmental and human microbiota, which can lead to immune dysfunction and impaired tolerance mechanisms 15.
On the other hand, we’ve known since 2005 that microbe-rich environments (living on a farm, close to nature, etc.) are associated with protection against immune diseases.
Beneficial effects of the exposome
“Environmental factors” are often associated with “adverse health effects”. But let’s not forget that part of the exposome is beneficial to our organism. According to a team of American and German researchers, exposure to daylight, green spaces, biodiversity, physical activity, social and emotional support, and a Mediterranean diet have all been shown to improve stress resilience, immune balance, and our circadian rhythm (body clock) 16.
To find out more, read our articles:
Fungal exposome: regulating the immune response
The microbiota, whether in the gut, vagina, lungs, or on our skin, comprises not only bacteria, but also viruses, archaea... and fungi. The fungal “mycobiota” is essential to the balance and stability of our microbiota. Numerous studies on infants have shown the microbiota fungal composition to be associated with the risk of developing an allergic disease.
Peanut allergy explosion: climate to blame?
In the US, peanut allergy in children increased by 21% between 2010 and 2017.
Is climate change to blame? This may well be the case, according to several studies showing that increases in CO2 and temperature are correlated with physiological changes in peanut plants. These may produce seeds with an altered antigenic profile that promote allergies 18.
We now know that the mycobiota largely depends on the fungal exposome. Analyses of fungal taxa have shown that the fungi most frequently found in the gut, mouth, lungs, and on the skin are the same as those found in the environment, whether indoors (walls, furniture, indoor air, etc.) or outdoors (food, water, soil, etc.).
Fungi present everywhere in the environment may therefore come into sustained contact with our organism, modulating our immune responses.
Do fungi in the nose play a role in rhinitis and asthma?
Drugs, exposome, microbiota: a delicate balance
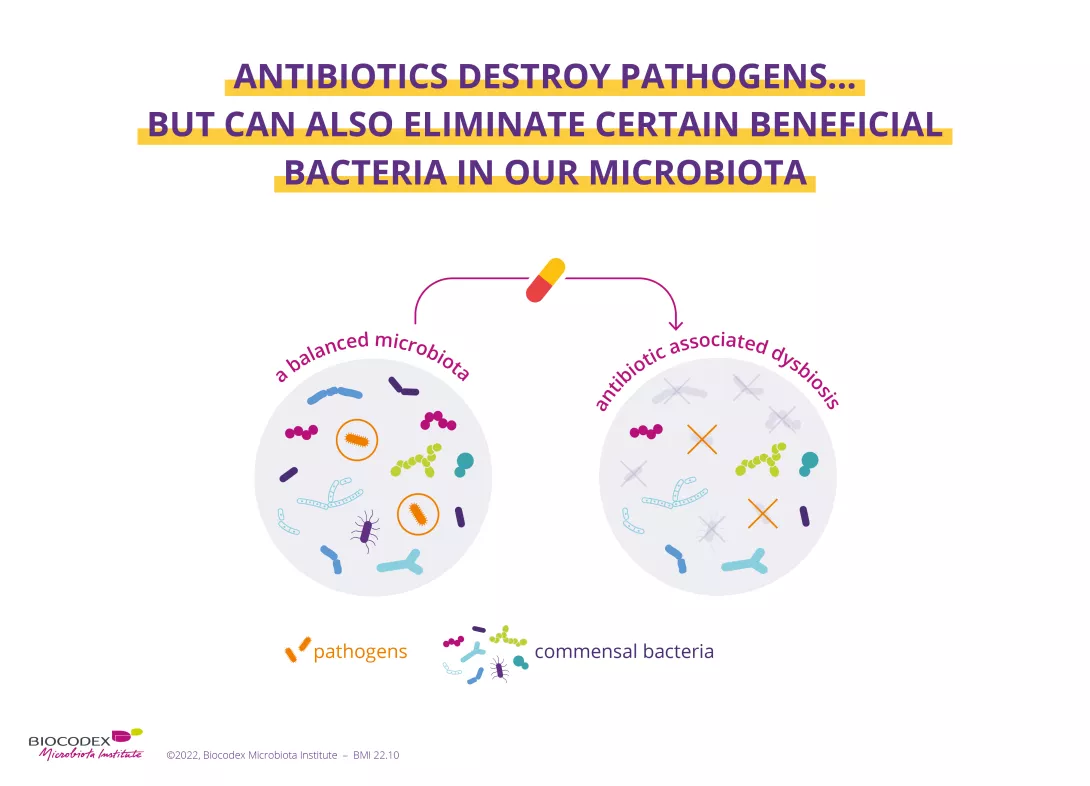
As part of our exposome, drugs interact in complex ways with the gut microbiota, influencing both its composition and functions.
Take, for example, common treatments such as proton pump inhibitors (PPIs), used to treat gastroesophageal reflux disease. PPIs modify the acidic environment of the stomach, allowing oral bacteria to reach the gut. This can influence the microbial ecosystem by favoring the growth of certain strains. These changes are associated with an increased risk of infection, such as those caused by Clostridium difficile, but can be controlled through appropriate use (avoiding long-term treatment where possible) and medical follow-up 20.
The microbiota is no mere bystander. It plays an active role in the processing of drugs.
For example, gut bacteria can improve the efficacy of metformin (an anti-diabetic drug) by stimulating the production of (sidenote: Short chain fatty acids (SCFA) Short chain fatty acids (SCFA) are a source of energy (fuel) for an individual’s cells. They interact with the immune system and are involved in communication between the intestine and the brain. Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. ) (SCFAs) beneficial to health.
Conversely, in rare cases, the microbiota can transform active molecules into toxic compounds, as in the case of brivudine, a now-banned antiviral used to treat shingels, which gut microorganisms can convert into liver-toxic bromovinyluracil.
These interactions highlight the importance of better understanding the relationships between drugs, microbiota, and exposome. By taking these mechanisms into account, we can optimize treatments and develop therapeutic strategies that respect and support the fragile balance of our gut ecosystem.
Read the rest of the article
Microbiota under pressure: how the exposome promotes chronic disease
Back to previous page
Exposome explained by our expert
1. Lionel Cavicchioli. Un organe sensible aux pollutions, Le Figaro Santé, avril-mai-juin 2024.
2. Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services (IPBES)
















