The gut microbiota is involved in the lung’s defense against viral respiratory infections
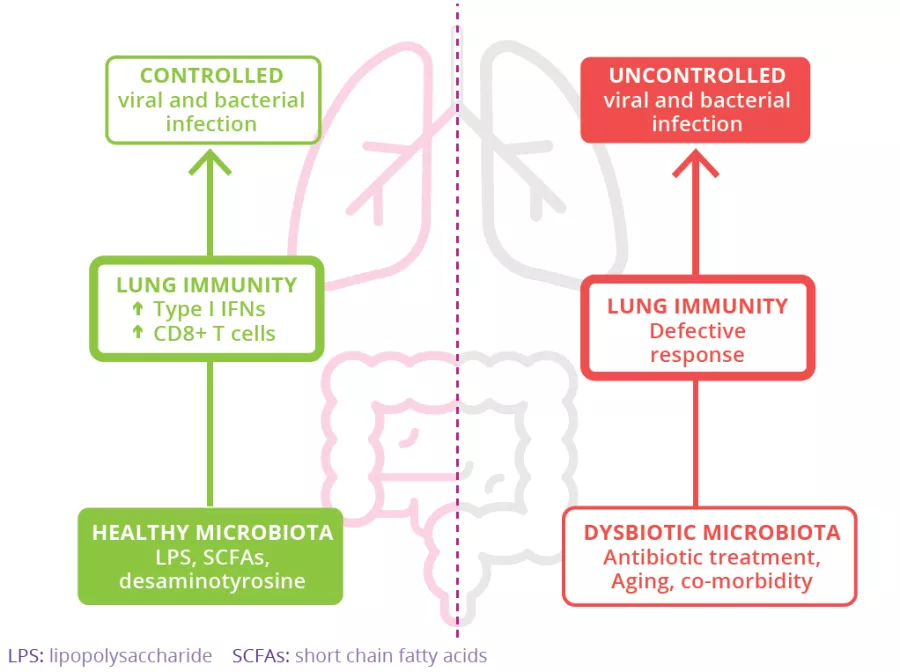
The microbiota plays a key role in the development, education and function of the immune system, both locally and systemically. While the airway microbiota locally regulates immune function, the gut microbiota can also influence respiratory immunity, via the gut-lung axis.1 Alteration of the lung and gut microbiota has been observed in many respiratory diseases, however whether the dysbiosis at these sites is a cause or a consequence of disease remains to be determined.2 Alteration of gut microbiota composition, through either diet, antibiotic use, aging, or disease, is associated with altered immune responses and homeostasis in the airways,3 highlighting that the gut microbiota can influence disease development throughout the body, including the risk of respiratory infections (Fig 6).4