What role does the microbiota play in the gut-brain axis?
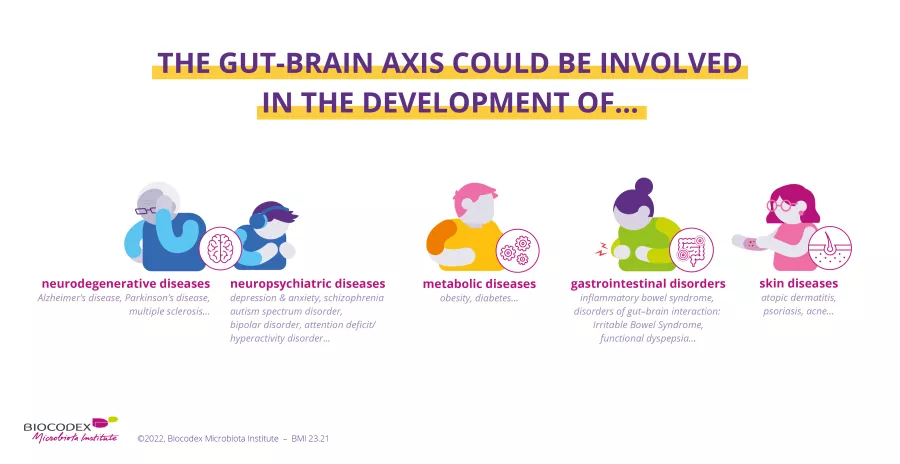
Known as our “second brain”, the gut takes part in a constant two-way dialogue with our real brain. This is known as the gut-brain axis. A breakdown in this axis may be involved in numerous gastrointestinal, metabolic, neurodegenerative, and neuropsychiatric disorders, as well as in certain skin diseases.
Here we tell you everything about the gut-brain axis, how it was discovered, the role played by the microbiota, how communication can be disrupted, and the associated diseases. And we also show you how to influence it.
- Learn all about microbiota
- Microbiota and related conditions
- Act on your microbiota
- Publications
- About the Institute
Healthcare professionals section
Find here your dedicated section
Sources
This article is based on scientific information

About this article
Table of contents
Table of contents
A little anatomy to begin
100 million The gut nervous system is thought to contain over 100 million neurons
The brain
The brain1,2 is a complex organ. In addition to integrating information from all parts of the body, it also controls thought, memory, emotions, touch, motor skills, vision, breathing, temperature, hunger, and all the mechanisms regulating our body. With the help of a wired network of 100 billion neurons, the brain acts as the body’s control center.
What is the nervous system?
The nervous system3 has two main parts:
- The central nervous system which includes the brain and the spinal cord.
- The peripheral nervous system which is made up of nerves that run from the spinal cord to all parts of the body.
The nervous system transmits signals between the brain and the rest of the body, including the internal organs.
The enteric nervous system (ENS), a “second brain” inside our gut4,5
The enteric nervous system (ENS) is the nervous system that governs the gut. Comprising a network of neurons that lines the walls of the gastrointestinal tract, it controls the sensory, motor, secretory, and immune activity of the digestive system.
Do you have butterflies in your stomach? Do you often have gut feelings? Or does reading this article get you in the gut? Many popular everyday expressions testify, without our knowing it, to the existence of a link between the gut and the brain.
Did you know?
The gut is sometimes called our second brain. But why?5,6
Because its nervous system is thought to contain over 100 million neurons, and it is very similar to the brain in terms of complexity and functionality (neurotransmitters and signal molecules).
The gut-brain axis through the years
The first documented report of a potential link between the gut and the brain dates back to the 19th century.7
The unintentional misadventures of a fur trader advanced science through the discovery of a connection between emotions and gut physiology8,9. Accidentally shot in the stomach at point-blank range, Alexis St. Martin was treated by US Army surgeon Dr. William Beaumont. Surgery had left the patient with an (sidenote: Fistula A fistula is an abnormal connection between an organ of the gastrointestinal system and the skin. ) and Dr. Beaumont took the opportunity to observe human digestion in the gut in real time.
During these observations he noticed that the patient’s digestive process was affected by his emotional state, i.e., whether he was angry or irritated. Beaumont thus discovered the existence of a brain-gut axis8. Further scientific studies showed communication between the gut and the brain to be a two-way process from gut to brain and brain to gut, and that the gut microbiota plays a key role in these exchanges8,10,11.
What is the gut-brain axis?
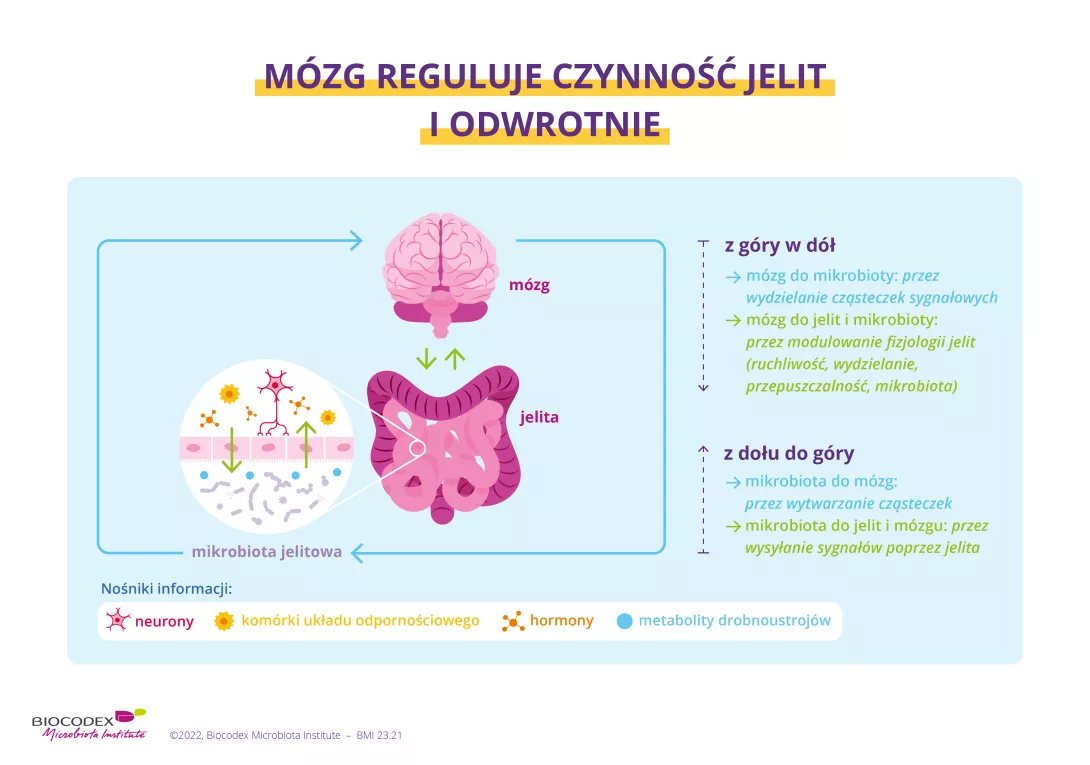
The gut-brain axis can be defined as a bidirectional communication network between the gut and the brain, with the former sending messages to the latter and vice versa. Communication takes place via three different channels8,12:
- the neuronal pathway (neurons), mainly via the vagus nerve and the enteric nervous system
- the endocrine pathway, through the secretion of hormones such as (sidenote: Cortisol Cortisol is known as the stress hormone. It plays a role in responses to physical and/or emotional stress. Cortisol is also involved in maintaining the balance of certain physiological functions, such as blood pressure, the immune system, the metabolism of proteins, carbohydrates, and fat, and anti-inflammatory action. Katsu Y, Iguchi T, Subchapter 95D - Cortisol. In Ando H, Kazuyoshi U, and Shinji N, eds. Handbook of hormones: comparative endocrinology for basic and clinical research. Pages 533-e95D-2 Academic Press, 2021. https://www.sciencedirect.com/science/article/abs/pii/B9780128010280002312 ) , (sidenote: Adrenaline Adrenaline, also known as epinephrine, is a hormone secreted by the adrenal glands and released into the bloodstream in the event of intense stress, danger, or strong emotions. It prepares the body to fight or flee from danger. https://my.clevelandclinic.org/health/body/23038-adrenaline ) , and serotonin
- the immune system pathway, through the modulation of cytokines
The gut-brain axis influences our behavior, cognition (memory), emotions, mood, desires, and perception, among other things.
90% Gut cells are responsible for over 90% of the serotonin production in the body
Did you know?
Serotonin is a neurotransmitter that can affect mood and feelings of happiness and pleasure, as well as appetite. Gut cells are responsible for over 90% of the serotonin production in the body8,13,14. The remaining 10% is produced by “serotonergic” neurons in the brain15. Certain bacteria in the gut microbiota may influence serotonin production in the gut8,16.
Does the microbiota play a role in the dialogue between gut and brain?
The microbiota can be considered the third player in the gut-brain axis, which is also known as the microbiota-gut-brain (MGB) axis.17
The brain, the gut, and the gut microbiota are the three nodes of the microbiota-gut-brain network. These nodes are interconnected and interact bidirectionally. The gut microbiota can communicate with the brain either directly by secreting signal molecules such as (sidenote: Neurotransmitters Specific molecules that enable communication between the neurons (the nerve cells in the brain), as well as with the bacteria in the microbiota. They are produced by the individual’s cells and by the bacteria in the microbiota. Baj A, Moro E, Bistoletti M, Orlandi V, Crema F, Giaroni C. Glutamatergic Signaling Along The Microbiota-Gut-Brain Axis. Int J Mol Sci. 2019;20(6):1482. ) or (sidenote: Short chain fatty acids (SGFA) Short chain fatty acids are a source of energy (fuel) for an individual’s cells. They interact with the immune system and are implicated in communication between the gut and the brain. Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. ) , or indirectly by interacting with gut cells as an intermediary. Similarly, the brain can modulate the microbiota. It can do so either directly or indirectly by modulating gut physiology in order to alter the microbial environment.
What factors influence communication between the gut and the brain?
Many factors are known to affect the dialogue between the gut and the brain:8
- Diet, and in particular certain foods,such as chocolate, can regulate our mood. The Mediterranean diet is also renowned for its beneficial effects on memory and health. Be careful what you eat. Limit your consumption of processed foods rich in additives, which, according to a recent study on rodents, may cause certain psycho-behavioral disorders (anxiety, reduced sociability, etc.).
- Regular physical activity has many beneficial effects on our health. Physical activity also contributes to good brain health. Numerous scientific studies have shown there to be a link between our cognitive system and our level of physical activity.
- Social interactions with family and those we live with stimulate the gut-brain axis. On the other hand, discrimination may be detrimental to the proper functioning of the gut-brain axis.
- The environment in which we live also has a major impact on our health and microbiota. Pollution is said to increase the risk of respiratory diseases, cancer, and cognitive disorders.
- Some drugs, especially antibiotics, may influence the development of a child’s nervous system and contribute to certain illnesses.
- Scientific studies have shown that the first years of life and the mode of delivery strongly impact our child’s microbiota and thus the gut-brain axis. In fact, several studies have linked cesarean birth to an increased risk of developing a variety of disorders, including obesity and immune system disorders such as asthma or allergies.8 Prenatal stress may also impact a child’s microbiota composition and neurological development, as well as the pregnancy itself, by increasing the risk of premature birth.18
- Stress and fear are also behavioral factors that affect our microbiota and the gut-brain axis.
- Is our behavior also linked to our microbiota? Certain studies suggest so…A healthy microbiota is a prerequisite for good emotional health, drives our libido and sexual desire while in some cases influence our addictive behaviors...
- Whatever your age, your gut microbiota will also influence your sleep and circadian rhythm.
What happens when communication between the gut and the brain is impaired
Disruption of the gut-brain axis is thought to be involved in a range of disorders.
By disruption we mean poor communication between the brain and the gut: either the signals sent are incorrect, or the messages are misunderstood or over-interpreted... In short, the gut and the brain no longer understand each other. Research is advancing our understanding of the gut-brain axis and pointing to the involvement of the gut microbiota in a growing list of diseases.8,17
Below is a non-exhaustive list of pathologies in which a disturbance of the gut-brain axis is thought to be involved.
Let’s take a closer look at some of these disorders:
GASTROINTESTINAL DISORDERS
Irritable bowel syndrome (IBS), formerly known as “functional bowel disorder”, is the most common disorder of the gut-brain axis. It is characterized by recurrent abdominal pain, bloating, bowel dysfunction, and other symptoms.
Functional dyspepsia is a kind of chronic indigestion – a stomachache, a feeling of fullness or bloating during and after meals. It too is a disorder of gut-brain interaction.19,20
Recent studies have shown the involvement of the gut-brain axis in inflammatory bowel disease (IBD)21,22, with the former potentially influencing both disease development and mental health.
METABOLIC DISORDERS
Type 2 diabetes mellitus (T2DM) is characterized by a chronic excess of sugar in the blood (hyperglycemia) linked to a malfunction in the production or use of insulin, the hormone that regulates blood sugar levels. Cognitive decline is one complication of type 2 diabetes.23
These pathologies (obesity, excess weight, metabolic syndrome) are often accompanied by psychological disorders such as anxiety, depression, bipolar disorder, or behavioral alterations.8
The microbiota may also influence what we put on our plate, our feeling of satiety24 as well as our eating habits. Recent studies have shown the role played by the gut microbiota and the gut-brain axis in eating disorders (disturbances in eating or eating-related behavior)25,26
Anorexia nervosa27,28 is an eating disorder that affects 1% of the population, with women making up 95% of those suffering from the disease. An imbalance of the gut microbiota is thought to contribute to the development and persistence of disorders related to the illness, such as loss of weight and appetite, by acting on the gut-brain axis and the metabolism.
Certain bacteria in the gut microbiota, such as Roseburia, are thought to be absent in anorexia nervosa patients.
Want to know whether your microbiota influences your waistline?
NEUROPSYCHIATRIC DISEASES
Psychiatric illnesses encompass a wide range of mental disorders, with imbalances in the gut microbiota shown to play a role in several of them.
Anxiety disorders29,30,31 are defined by the WHO as excessive fear and worry as well as related behavioral disorders. Symptoms are severe enough to cause significant distress or major functional impairment. Some anxiety disorders may be linked to the activity of the gut microbiota through the regulation of stress hormones.
Depression, bipolar disorder, etc. Mood disorders8,32 are emotional disturbances that involve long periods of excessive sadness (depression), excessive cheerfulness or elation (mania), or both of these.
Depression and bipolar disorders have been linked to a gut dysbiosis, with the dysbiosis sometimes correlated with the severity of the symptoms.
Other studies have gone even further by using the gut microbiota as a diagnostic tool.
Obsessive-compulsive disorder (OCD)33,34,35 is a neuropsychiatric disorder affecting 1.3% of the general population. The disorder is characterized by obsessions (repeated, persistent, unwanted, and often anxiety-provoking ideas or images) which lead to repetitive and time-consuming compulsions and/or avoidance behaviors designed to neutralize the anxiety and anguish resulting from the obsessions. Some studies have suggested that certain butyrate-producing bacteria are less abundant in OCD patients.
Schizophrenia8,36,37 affects around 1 in 300 people. This psychiatric illness is characterized by delirium and hallucinations, social isolation, and psychological disruption. Disturbances of the gut microbiota and the immune system are thought to be involved.
Autism spectrum disorders (ASD)38 are a heterogeneous group of disorders associated with brain development abnormalities. Symptoms include deficits in communication, social interaction and behavior disorders, as well as repetitive behaviors.
Some studies have shown an altered gut flora (dysbiosis) to be common in autistic patients and certain gut disorders (diarrhea, constipation, etc.) to be frequently associated with the disease.
Gut dysbiosis is thus involved in many psychiatric illnesses such as schizophrenia, depression, and obsessive-compulsive disorder (OCD).
But does each illness have its own specific dysbiosis or are there common microbial changes?
Find out more about the gut microbiota’s role in the onset of mental disorders via the gut-brain axis
NEURODEGENERATIVE DISEASES
Neurodegenerative diseases are characterized by the gradual destruction of certain neurons.
Alzheimer’s disease39,40 is the most common neurodegenerative disorder and the leading cause of dementia.
In recent years, the gut microbiota has been the subject of interest, particularly certain proteins (amyloid peptides) produced by “harmful” bacteria, which may trigger an inflammatory mechanism and disrupt the barrier functions of the gut and the brain, thereby promoting the development of the disease.
Parkinson’s disease41 is a neurodegenerative disorder that progressively destroys the dopamine neurons in the brain. The disease is characterized by slowness in movements, muscle rigidity, and tremors.
A link to a disruption in the gut microbiota and the gut-brain axis has been shown.
Multiple sclerosis42,43 is an inflammatory disease of the central nervous system. It is characterized by an “autoimmune response”, whereby the immune system attacks the protective myelin sheath surrounding the neurons. This inflammation leads to a degeneration of nerve cells, or neurons, and a loss of communication between the brain and peripheral organs.
Recent studies have suggested specific associations between the gut microbiota and the risk of multiple sclerosis, its progression and outcome.44
A gut-brain-skin axis?
Did you know?
You may not know it, but the gut and skin have many common features45: both contain numerous blood vessels and nerve connections, both interact with the immune system, and of course both are massively colonized by microbial communities. But that’s not all... have you noticed how your skin reacts to your emotions? Music, fear, excitement... The same applies to certain skin diseases when the gut, the skin, and the brain no longer communicate properly.
As early as 1930, dermatologists John Stokes and Donald Pillsbury46 suggested that emotional states such as anxiety or depression could alter the gut microbiota and induce local or systemic inflammation in other organs such as the skin.47 They recommended the use of fermented milk to reintroduce beneficial microorganisms.
Recent years have seen growing evidence for a link between the gut, the brain, and the skin.48 More precisely, stress leads to the secretion of hormones (serotonin, cortisol, etc.), which in turn increase gut permeability, causing local inflammation, while also provoking systemic inflammation via the bloodstream.11,23 Ultimately, this is thought to impact the skin barrier and cause skin inflammation.25 This gut-brain-skin axis is thought to be involved in certain skin diseases: Acne, Atopic dermatitis and Psoriasis
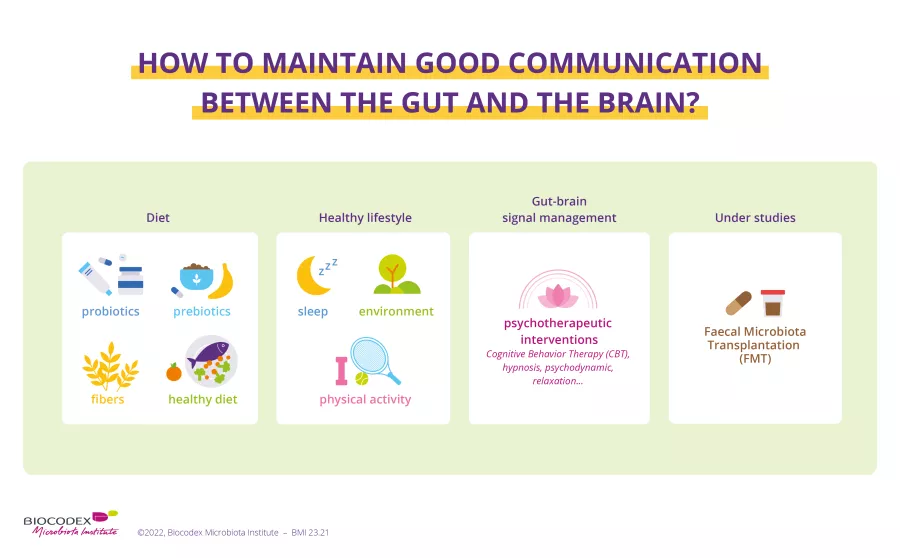
How can we ensure good communication between the gut and the brain?
By now the gut-brain axis is no secret to you. The two-way dialogue exists from gut to brain and brain to gut, with the gut microbiota in between.
But how can we take care of our microbiota so that messages are sent and received loud and clear?
Numerous scientific studies have looked at how to avoid any disruption to microbial composition and how best to preserve its balance49.
Diet:
What we eat contributes to the balance of our gut microbiota.50,51 The food we eat is beneficial when varied and of good quality, but an unbalanced diet can affect the composition of our gut microbiota and lead to certain diseases.52 It is therefore important to know which types of food have positive effects on our health53. These include fermented foods or foods naturally rich in prebiotics and beneficial microorganisms, some of which will impact our mental health. These foods may have the ability to boost our morale by acting on the brain via the gut microbiota.54
Want to know more about the foods that benefit our health and the role of the gut microbiota?
=> Includes an interview with Professor Rémy Burcelin who has studied the mechanisms at work between the brain, the gut, and the rest of the body.
What is a psychobiotic?
Psychobiotics are probiotics and prebiotics which, when ingested, provide mental health benefits via the gut microbiota.55
Researchers at University College Cork in Ireland have suggested broadening the definition of psychobiotics beyond probiotics and prebiotics to include any substance that exerts a psychological effect mediated via the gut flora.56
Probiotics:
Probiotics are live micro-organisms which, when administered in appropriate quantities, benefit the health of the individual57,58. Some non-clinical and clinical studies have focused on the administration of probiotics to improve symptoms of stress, anxiety, and depression, with results showing promising beneficial effects.8
Prebiotics:
Prebiotics are specific non-digestible dietary fibers with health benefits. They are selectively used by beneficial microorganisms in the host microbiota.59,60 Studies have shown that certain prebiotics have beneficial effects on stress-related disorders.8
Transplant:
To restore the balance of the gut’s microbial ecosystem, patients can be given a fecal microbiota transplant (FMT) from a healthy donor.61 For the moment, this therapeutic approach has only been approved for the treatment of recurrent Clostridioides difficile62 infections, but researchers have expressed considerable interest in it and are assessing its impact on addictions such as alcoholism63 or even on gut-brain interaction disorders such as irritable bowel syndrome.64,65
Psychotherapeutic interventions
(sidenote: Mind-body therapies Mind-body therapies are practices that focus on the relationships between the body, brain, mind and behavior and their effects on health and disease. Wahbeh H, Elsas SM, Oken BS. Mind-body interventions: applications in neurology. Neurology. 2008;70(24):2321-2328 ) have been shown to have beneficial effects on mental health in the management of stress and gut-brain interaction disorders such as IBS: (sidenote: Cognitive-behavioral therapy A type of psychotherapy where therapists help patients to identify the impact of their dysfunctional thoughts (incorrect, negative) on their behavior and well-being. Cuijpers P, Smit F, Bohlmeijer E, et al. Efficacy of cognitive–behavioural therapy and other psychological treatments for adult depression: meta-analytic study of publication bias. The British Journal of Psychiatry. 2010;196(3):173-178 InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006. Cognitive behavioral therapy. 2013 Aug 7 [Updated 2016 Sep 8] ) , hypnosis, meditation, relaxation, (sidenote: Biofeedback A method for learning how to control certain bodily functions, such as heart rate, blood pressure and muscle tension, using a special device. It can help control pain. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/biofeedback ) ...66
Recommended by our community

"An interesting read" -George Lewis (From My health, my microbiota)
"I need to know more about this. This may be what’s going on. " -Mark Chadney (From My health, my microbiota)
1. Central nervous system (CNS) https://www.healthdirect.gov.au/central-nervous-system
2. https://institutducerveau-icm.org/fr/actualite/comprendre-le-cerveau-et-son-fonctionnement/
3. MedlinePlus. (2016). Neurosciences. Retrieved august 16, 2023
15. https://my.clevelandclinic.org/health/articles/22572-serotonin/
17. Mayer EA, Nance K, Chen S. The Gut-Brain Axis. Annu Rev Med. 2022;73:439-453.
19. https://my.clevelandclinic.org/health/diseases/22248-functional-dyspepsia
30. https://www.who.int/news-room/fact-sheets/detail/mental-disorders
32. https://www.msdmanuals.com/home/mental-health-disorders/mood-disorders/overview-of-mood-disorders
37. https://www.who.int/news-room/fact-sheets/detail/schizophrenia
42. https://institutducerveau-icm.org/en/multiple-sclerosis/