Although limited in immunosuppressed patients because of an increased infectious risk, the use of prebiotics or probiotics and fecal microbiota transplant (FMT) can have significant benefits for patients who underwent HSCT. Combined to new techniques to analyze, characterize and monitor the gut microbiota, this use could transform the prevention of infections and graft rejection.
In a study with 30 children and adolescents, the use of probiotics, especially a Lactobacillus species, during the antibiotic prophylaxis phase or the follow-up phase of HSCT, prevented the onset of GVHD in 70% of cases, with no subsequent Lactobacillus bacteremia.13 Regarding FMT, its safety and beneficial effects against C. difficile infection were recently proven on small cohorts of patients who underwent HSCT:13 in one trial, fecal transplants led to remission in 3 out of 4 cases, and in another study, it led to a decrease of symptoms in GVHD after several grafts. The microbiota of antibiotic-treated patients who received an autologous fecal microbiota transplant was restored on D+100 following the HSCT.16 Some scientists thus suggest performing FMT before HSCT in patients carrying C. difficile-resistant strains.
DIET AND PROBIOTICS
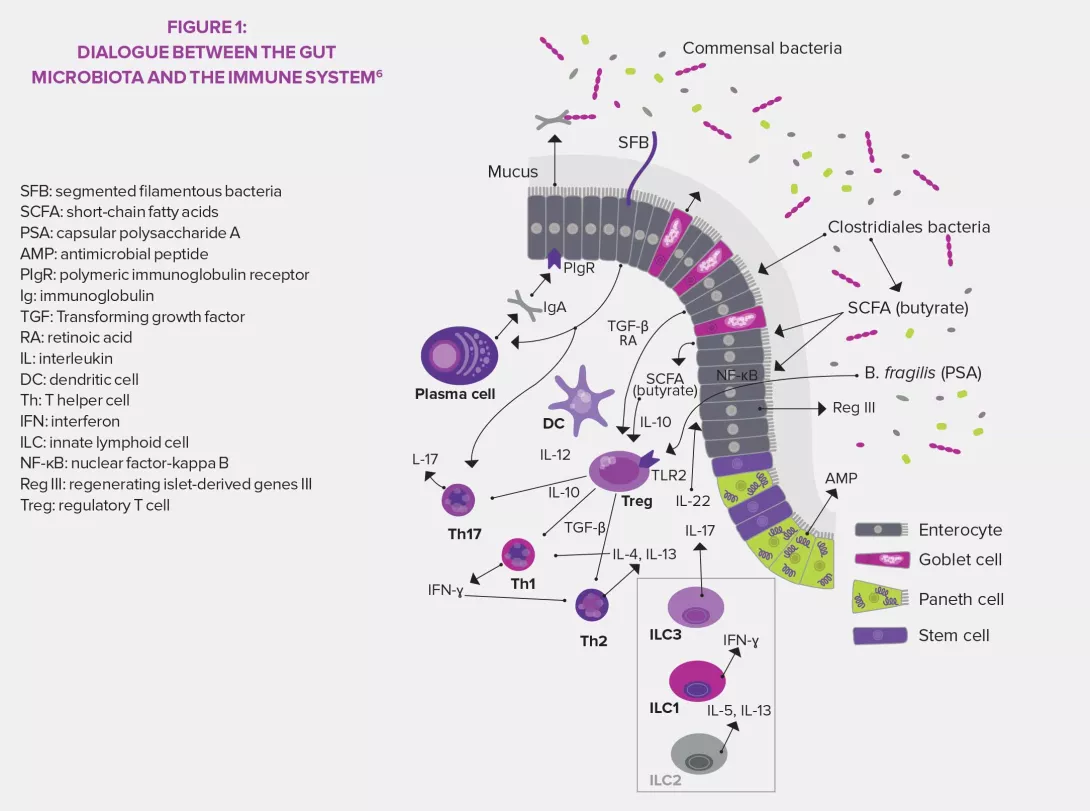
Short-chain fatty acids (such as butyrate) have shown positive effects against GVHD. They serve as energy source as well as anti-apoptotic agents for enterocytes, and they have an anti-inflammatory action by promoting the synthesis of Treg. Beneficial effects on the intestinal mucosa were observed on other components metabolized by the gastrointestinal microbiota: indole derivatives produced by the fermentation of Brassicaceae (cabbage, broccolis…), tryptophan (dairy products, banana…),17 bile acids. The association of fiber, glutamine and oligosaccharides reduced morbimortality in 44 transplant patients. A trial is currently ongoing regarding the benefits of resistant starch, a prebiotic that promotes the production of butyrate.12
OTHER INNOVATIONS UNDER DEVELOPMENT
The therapeutic arsenal could also be broadened by innovations such as targeted antibiotic therapy that aims at limiting the destruction of the digestive barrier and the emergence of multidrug resistant bacteria (antibiotics guided by pathogen-specific antibodies or synthetic bacteria that compete with pathogens are currently under trial). Thanks to new technologies, we are able to recreate in vitro interactions that occur in vivo within the gastrointestinal microbiota. As for bacterial profiling tools, they open the way to personalized medicine adapted to the microbiota of each patient in order to choose the most adequate therapeutic protocol.12