Among other factors is, once again, gut dysbiosis! It leads to an increase of intestinal permeability and a disruption of stress response, as well as an increase in inflammatory activity.
All roads lead to the microbiota15
Scientists agree that gut bacteria play a role in this process. But according to scientific studies, the microbiota could either have an anxiety-inducing effect or an anxiolytic effect16. The use of antibiotics– that disrupt and impoverish the gastrointestinal flora–could be associated to the onset of anxiety disorders, or conversely, to a decrease in anxiety in animals.
The flora is being explored “blindly”
In animal models, antibiotics seem to decrease anxiety during the treatment period. The drawback is that an early disruption of the gut microbiota by antibiotics could lead to behavioral changes that persist into adulthood17,18. Some probiotic strains could also have an anxiolytic effect. Finally, fecal microbiota transplant could reduce anxiety levels19. All these results still have to be confirmed in humans.
What to eat to stay zen?
Fermented foods such as cheese, yogurts, kefir, kombucha or soy sauce are excellent sources of probiotics and prebiotics. They act as anti-inflammatory agents by strengthening the integrity of the intestinal barrier, improving the composition and function of gut bacteria, and stimulating immune cells in the digestive tract. Probiotics decrease frequency and severity of anxiety symptoms in rat models. In humans, they decrease cortisol levels in urine21. In healthy people with no psychiatric disorders, consumption of fermented milk leads to changes in brain activity in regions that are responsible for emotions and pain.
Healing - Body and mind20
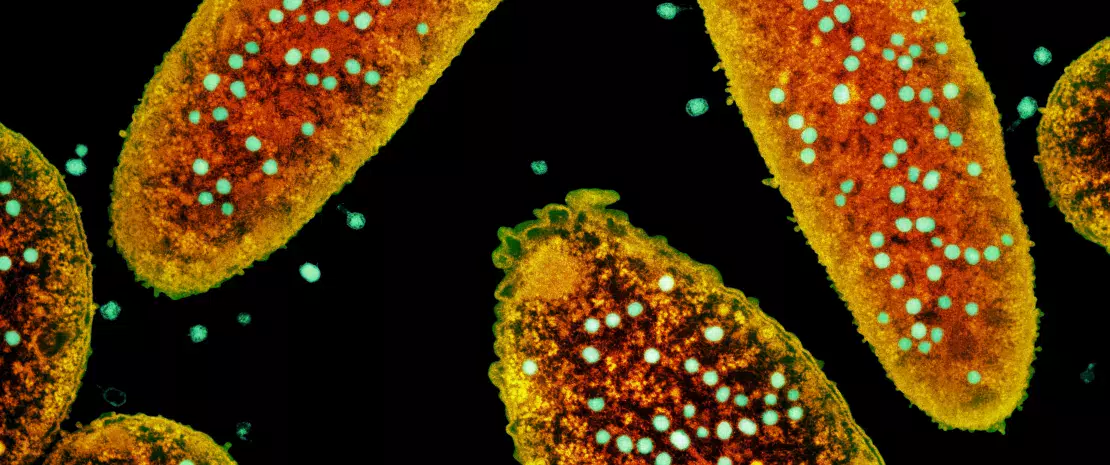
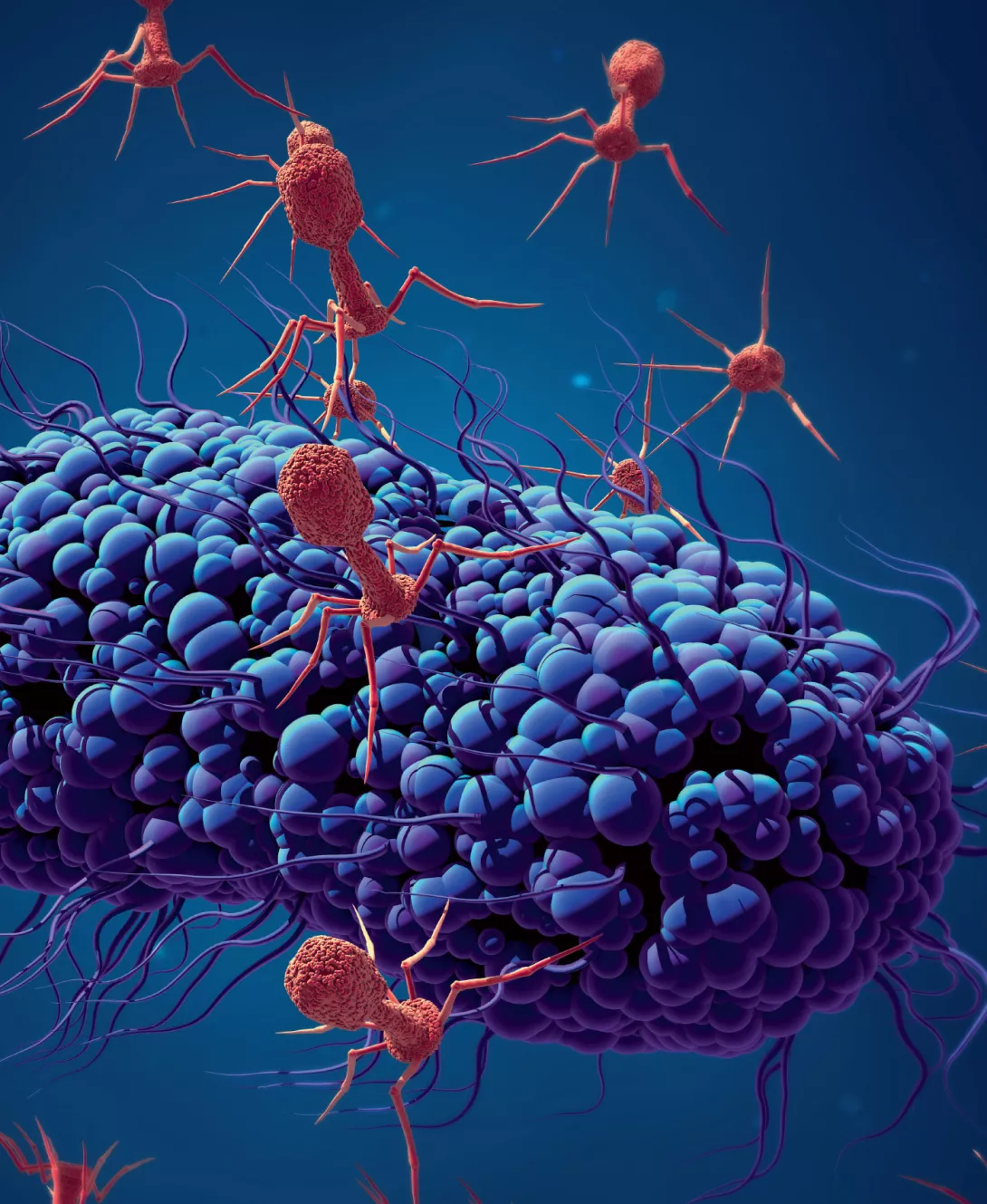
Psychobiotics are live microorganisms (bacteria, for instance) which, once ingested, produce a beneficial effect on the health of patients with psychiatric, psychological or neurological disorders.
In brief, they are probiotics that could have psychotropic properties and regulate the gut-brain axis by: