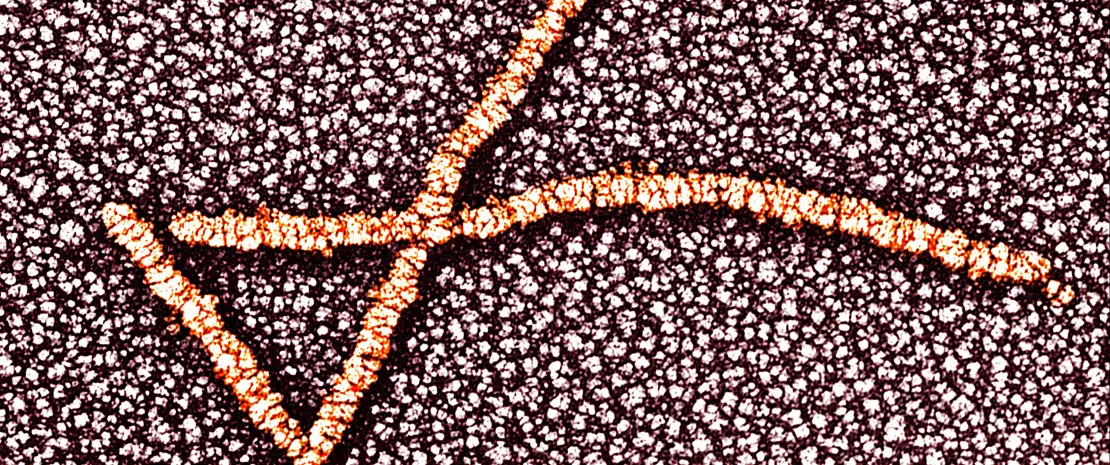
The composition of the vaginal microbiota changes throughout women’s lives: while it has a particularly low content of Gardnerella vaginalis, Prevotella and lactobacilli before puberty, it becomes almost exclusively colonized by lactobacilli after puberty. Lactobacilli ensure women’s health by fighting against pathogens. Their decrease is associated to various gynecological disorders, such as premature delivery, infertility, sexually transmitted infections or even pelvic inflammatory diseases. Shortly before menopause, hormonal variations cause significant changes in the composition of the vaginal microbiota which finds a different balance after menopause.
Microbes and reproduction
Vaginal microbiota also seems to play a role in conception, whether it is natural or by means of in vitro fertilization (IVF). The presence of Gardnerella vaginalis and Atopobium vaginae in the vaginal microbiota was associated to lower success rates, while treatment of bacterial vaginosis, which is frequent in infertile women, improves pregnancy rate. Success also depends on the proportion of lactobacilli in seminal fluids as well as the presence of some species in the Fallopian tubes and the uterine mucosa (endometrium), whose microbiota could either favor or limit chances of embryo implantation.
The baby’s health starts in the uterus
The baby’s immune and metabolic systems could be determined during intrauterine life through its exposure to maternal microbes which are present in the placenta and amniotic liquid and can also be found in the newborn’s first stools (meconium). At present, it is unknown if the placenta hosts its own microbiota. It is known however, that it is similar to the maternal oral flora, which could explain why pregnant women with periodontal diseases have an increased risk of facing pregnancy-related complications. Moreover, changes in its composition are associated to premature births.
Risks and benefits
Although the mother is a source of microbes for her baby, other factors come into play to modulate the baby’s microbiota. Use of antibiotics by the mother (especially in the second or third trimesters of pregnancy) as well as cesarean delivery (because the newborn does not come into contact with the mother’s vaginal microbiota) are associated with an increased risk of childhood obesity. On the contrary, probiotics seem to benefit the mother and her unborn child, according to the researcher Jessica Younes. In pregnant women, they could reduce the risk of premature delivery, gestational diabetes, postpartum depression or urinary and vaginal infections; whereas in the newborn child they could limit colic, predisposition to developing allergies (atopy), resistance to antibiotics and could also reduce— or even eliminate—the risk of necrotizing enterocolitis which is a fatal disease. Finally, breastfeeding or formula feeding could play a significant role in the child’s microbiota composition, although its impact on childhood health remains unknown.