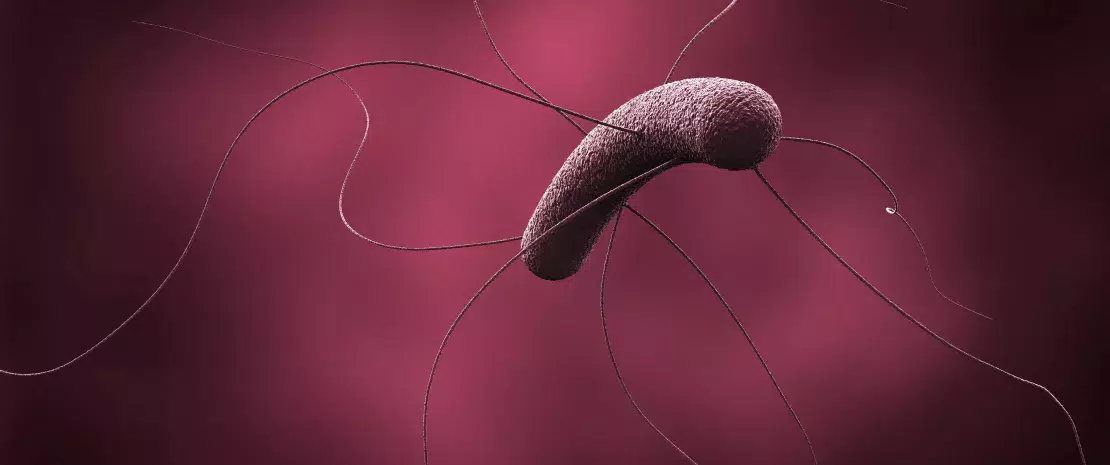
As the impact of the gut microbiota on our health is increasingly better documented, strategies able to favorably affect it are being developed, particularly through diet. Some researchers thus focus on foods specifically aimed at acting on the microbiota, or MDF (microbiota-directed foods), in this case, polysaccharides (plant fibers).
34 “fibers” were analyzed
A murine model led to a better understanding of how human gut bacteria interact with dietary polysaccharides, as well as with each other: germ-free mice colonized by beneficial gut bacterial strains (Bacteroides spp. from a slim adult male, that distinguish him from his obese twin) were fed different combination of 34 dietary fibers, in addition to a fiber low diet (representative of the typical American diet). By combining several cutting-edge technologies, the researchers identified the fiber bioactive compounds that promote the development of some Bacteroides species. Twenty-one out of 34 tested polysaccharides significantly improved the growth of some species, such as citrus pectin and pea fiber with Bacteroides thetaiotaomicron. These results could eventually allow us to increase the content of these active compounds in our diet.
Inter-species competitions
To understand the mechanisms at play and identify the fibers that are ingested or not, additional experiments were carried out using biosensors, i.e. magnetic beads coated with polysaccharides and easily recovered in the stools. They confirmed that 2 different bacterial species (for instance Bacteroides cellulosilyticus and Bacteroides vulgatus) are able to degrade the same polysaccharide, as long as they are equipped with the necessary genes. As a result, different strains compete for nutritional resources.
Towards personalized nutritional medicine?
By analyzing how gut microorganisms adapt to their environment (by counterbalancing the absence of a specific species or by competing with each other), the scientists observed that some bacteria were more flexible than others, as regards the use of the substrate. This is the case for Bacteroides ovatus, which is able to adapt to the presence of B. cellulosilyticus, its competitor for arabinoxylan (a major component of plant cell walls in cereals and peas), while B. vulgatus does not have this ability. Identifying which organisms are the most flexible helps us understand how some strains can coexist with the other “inhabitants” of the gut community. Based on these results, the team already foresees the development of personalized dietary guidelines based on microbiological and physiological data from the host obtained with biosensors.