Breast milk is not sterile and the flora it hosts contributes to the development of newborns’ gut microbiota. But are all breast milk feeding techniques equally effective? To find out, an international team analyzed the composition of breast milk microbiota, either pumped or given directly from the breast, in 393 new mothers.
Impact of using a breast pump
The microbial composition of 393 breast milk samples, collected on average 3-4 months after birth, was matched to the breastfeeding mode of each mother and specific parameters (BMI, parity, delivery mode...) using several statistical methods. Bifidobacterium spp., bacteria involved in the maturation of the child’s immune system, were more abundant in the milk when it was given directly from the breast. Independently of other factors traditionally considered (mother BMI, delivery mode...), expressed breast milk feeding (defined as at least one feed with expressed milk in the previous two weeks), and especially with an electric breast pump, significantly reduced abundance and diversity of the milk’s microbiota. It also induced an increase in several families such as Enterobacteriaceae, Enterococcaceae, Stenotrophomonas and Pseudomonadaceae, of which some species are potential opportunistic bacteria. This observation suggests that environmental factors impact indirect breastfeeding.
Other factors to be considered
Results also indicate that in case of direct breastfeeding, the newborn itself regurgitates and contaminates the milk with its own oral microbiota (“retrograde inoculation” hypothesis), in a gender-specific manner. This is an additional argument supporting the idea of a shared mother-child contamination. Similarly, maternal factors could have an impact: ethnicity, BMI (able to modulate, among others, the amounts of fatty acids, hormones or oligosaccharides in the milk), delivery via C section (leading to decreased bacterial diversity and abundance in the milk), smoking, primiparity or multiparity, existence of an atopic field. And let’s not forget translocation of gut microorganisms towards the mammary glands, through the “entero-mammary pathway”. These findings could lead to potential avenues to improve milk microbiota, and consequently newborns’ intestinal flora, and implement prevention strategies for chronic diseases from an early age (allergies, respiratory infections. asthma...).

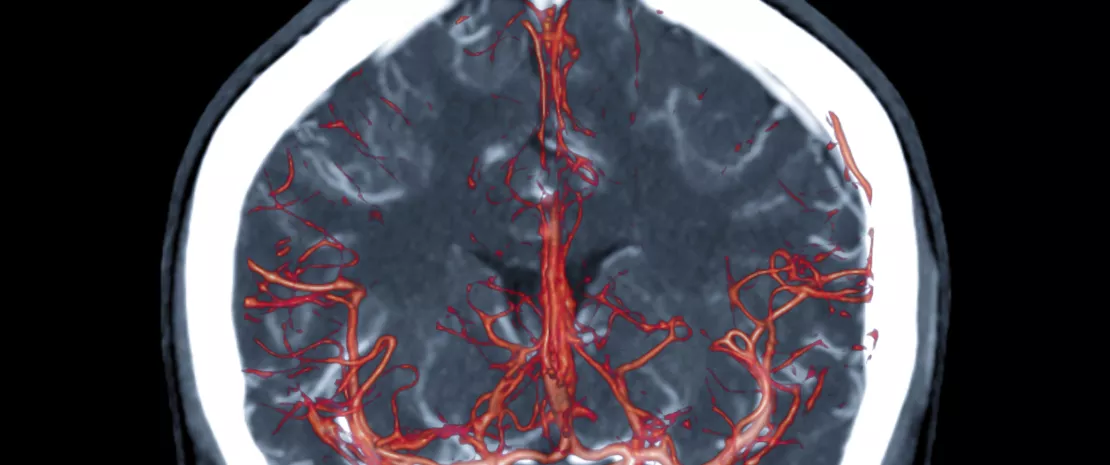
 Show me your gut flora, and i’ll tell you where you come from
Show me your gut flora, and i’ll tell you where you come from
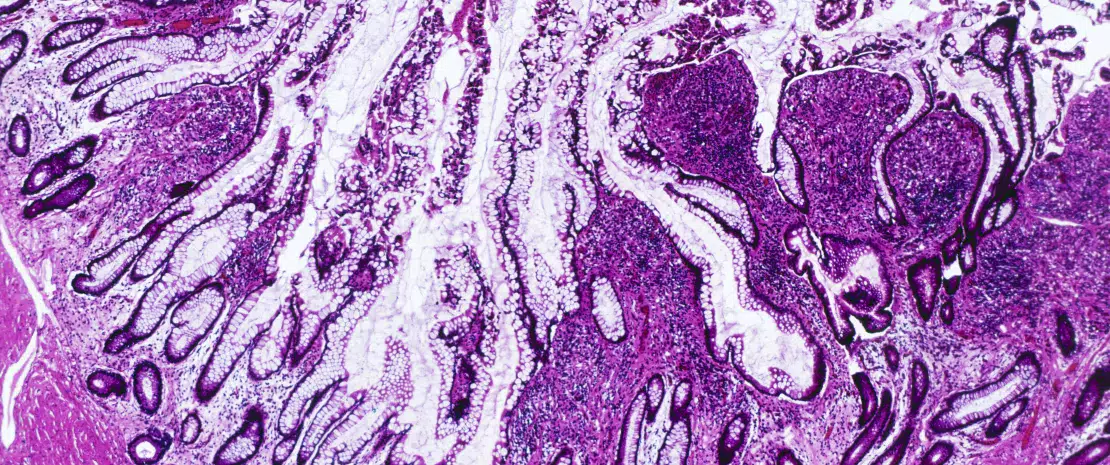
 MICROREVEAL no. 2: A closer look at intestinal microbiota
MICROREVEAL no. 2: A closer look at intestinal microbiota