International Microbiota Observatory: Focus on women health 2024
Only one in five women claim to know exactly what the “vaginal microbiota” is
The vaginal microbiota is essential to women's health. But how well known is it among women? What behaviors do they adopt to protect it? What information do they receive from their healthcare professionals? How have knowledge and attitudes about the vaginal microbiota changed since last year?

For the second year running, the Biocodex Microbiota Institute has commissioned Ipsos to conduct a major international survey on the microbiota:
The International Microbiota Observatory. The survey was conducted by Ipsos among 7,500 people in 11 countries (France, Spain, Portugal, Poland, Finland, Morocco, United States, Brazil, Mexico, China, and Vietnam). In each country, the sample surveyed is representative of the country's population aged 18 and over in terms of gender, age, occupation, and region. The survey was conducted over the Internet between January 26 and February 26, 2024.
The second wave of this study once again highlights women’s lack of awareness about the vaginal microbiota, which remains largely unknown. However, the study also indicates that knowledge and behaviors are improving this year, thanks to more widespread education from healthcare professionals. This education must now be reinforced and extended to all women, especially older women.
The vaginal microbiota is still poorly understood, although knowledge is slightly better this year
- Once again this year, only one in five women claim to know exactly what the “vaginal microbiota” is (22%, +2 points vs. 2023, vs. 20% men and women combined). Awareness of the term is greater compared to last year, but remains low: nearly half of women have still never heard of it (48%, -5 points vs. 2023, vs. 51% of men and women combined).
- Women are more familiar with the term “vaginal flora”, even if knowledge of the term remains superficial: only one woman in two knows exactly what it is (53% vs. 42% for men and women combined).
- A degree of good knowledge about certain characteristics of the vaginal microbiota: almost 7 out of 10 women know that antibiotics can alter the vaginal microbiota (69%) and that vaginal dryness/dehydration has consequences for the vaginal microbiota (69%).
- Knowledge is still too weak, but improving on last year: 55% of women know that from childhood to menopause, a woman’s vaginal microbiota does not remain the same (+6 points vs. 2023), and 44% know that bacterial vaginosis is associated with an imbalance in the vaginal microbiota (+8 points vs. 2023).
- However, knowledge about many aspects of the vaginal microbiota remains very limited: only 1 in 2 women knows that smoking has an impact on the vaginal microbiota (55%) and 3 in 10 women know that the vaginal microbiota is balanced when its bacterial diversity is low (30%; +2 points vs. 2023)
This year, more and more women are adopting behaviors aimed at protecting the vaginal microbiota, even if certain bad practices persist
- The adoption of behaviors to protect the vaginal microbiota varies: while women are very likely to wear cotton underwear (86%, +2 points vs. 2023), other beneficial behaviors are less common. Around 2 out of 3 women avoid self-medication (63%), and 3 out of 5 use a soap-free cleansing solution (61%, +3 points vs. 2023).
- Certain behaviors that are harmful to the vaginal microbiota remain ingrained: despite a reduction compared to last year, more than 2 out of 5 women still practice vaginal douching (42%, -3 points vs. 2023), and 53% sleep in their underwear (+1 point vs. 2023).
More education from healthcare professionals, which must be stepped up to meet women's needs
- Healthcare professionals delivered more education about the vaginal microbiota this year: 43% of women have received an explanation about the vaginal microbiota (+7 points vs. 2023). Nearly half of women have been made aware of the importance of protecting their vaginal microbiota as much as possible (+8 points vs. 2023). A similar proportion of women stated that a healthcare professional has explained the behaviors to adopt to protect their vaginal microbiota as much as possible (48%, +7 points vs. 2023). Although this progress is noteworthy, it only concerns a minority of women, illustrating room for improvement in the information passed on by healthcare professionals concerning the vaginal microbiota.
- This is especially true since women have been widely requesting this kind of awareness-raising. 88% would like to be better informed about the importance of the vaginal microbiota and its impact on health (+2 points vs. 2023).
2024: What women know (and don't know) about their vaginal microbiota
Age is a determining factor when it comes to the vaginal microbiota: people aged 60 and over are less aware, in contrast to 25-34 year-olds and young mothers
Once again this year, women aged 60 and over remain the least informed and aware of the vaginal microbiota, even though they are more exposed to health problems.
- Only 41% of women aged 60 and over know what the vaginal microbiota is, compared with 52% of women overall.
- They also lack knowledge of the role and functions of the vaginal microbiota: less than half of women aged 60 and over (49%) know that the vagina is self-cleaning (vs. 56% of all women), and only 39% know that bacterial vaginosis is associated with an imbalance in the vaginal microbiota (vs. 44% of all women).
- Despite these knowledge gaps, women aged 60 and over stand out for adopting certain behaviors aimed at preserving the balance of the vaginal microbiota. Thus, 3 out of 4 of them avoid relying on self-medication (76%, vs. 63% of all women) and 67% avoid practicing vaginal douching (vs. 58% of all women). However, fewer of the women aged 60 and over use a soap-free cleansing solution (56%, vs. 61% of all women) and sleep without underwear (43%, vs. 47% of all women).
- This population has received less education from healthcare professionals: only a third of women aged 60 and over have received an explanation about the vaginal microbiota from a healthcare professional (32%, vs. 43% of all women).
Women aged 25 to 34 and mothers of children under 3 appear to be more informed and aware of the vaginal microbiota.
- 62% of 25-34 year-olds and 60% of mothers of children under 3 know what the vaginal microbiota is (vs. 52% of all women).
- A better understanding of the vaginal microbiota: 69% of 25-34 year-olds and 67% of mothers know that every woman has a unique vaginal microbiota (vs. 64% of all women). More of these women also know that the vagina is self-cleaning: 61% of 25- 34 year-olds and 60% of mothers know this (vs. 56% of all women).
- More of these women have adopted certain behaviors that are beneficial for their vaginal microbiota: 2 out of 3 use a soap-free cleansing solution (67% of 25-34 yearolds and 71% of mothers of children under 3, vs. 61% of all women), and 54% sleep without underwear (vs. 47% of all women).
- 54% of 25-34 year-olds and 55% of mothers of children under 3 have received information from a healthcare professional about the vaginal microbiota (vs. 43% of all women).
The International Microbiota Observatory also revealed striking contrasts between countries in terms of knowledge, behaviors and information provided by healthcare professionals. The complete results are available on the Biocodex Microbiota Institute website.
The International Microbiota Observatory: what is it ?
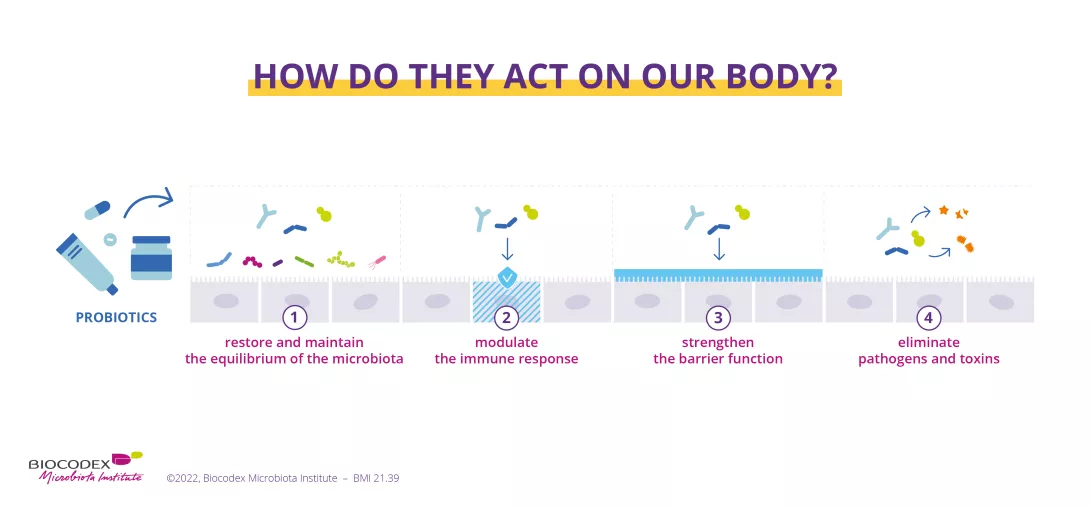
About the Biocodex Microbiota Institute
The Biocodex Microbiota Institute is an international knowledge hub dedicated to human microbiotas. Available in 7 languages, the Institute is aimed at both healthcare professionals and the general public, to raise awareness of the vital role that this part of the body plays in our health. The primary mission of the Biocodex Microbiota Institute is educational: to promote the importance of the microbiota for everyone.
Contact us
Biocodex Microbiota Institute press contact:
Olivier VALCKE
Public Relations and Editorial Manager
+33 6 43 61 32 58
o.valcke@biocodex.com
Ipsos press contact:
Etienne Mercier
Director of the Opinion and Health Division - Ipsos
+33 6 23 05 05 17
etienne.mercier@ipsos.com
BMI-24.21