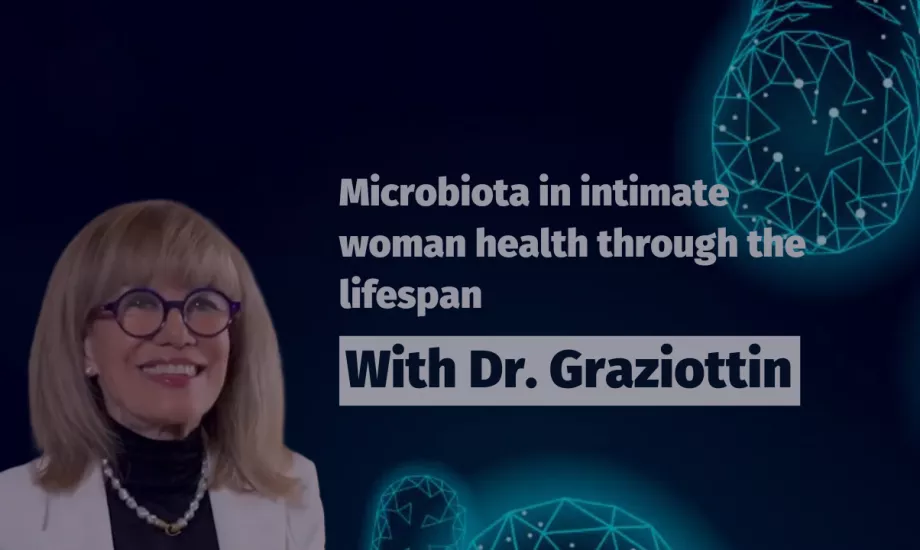
Xpeer course: Microbiota in intimate woman health through the lifespan
Gynecologists, midwives, and pharmacists, get free training on "Microbiota in intimate woman health through the lifespan" from Professor Alessandra Graziottin in this CME course.
Synopsis of the course
This accredited course aims to educate gynecologists, midwives, and pharmacists on the significance of microbiota, particularly vaginal microbiota, for intimate health. Led by a renowned expert, Dr. Graziottin, thoroughout the course participants will gain a comprehensive understanding of how microbiota impacts intimate health across the lifespan. We will first cover the basic insights about the gut microbiome before delving into the vaginal microbiota throughout different life stages, including the potential for a sterile placenta, neonatal microbiota, and changes during infancy, puberty, fertile years, and menopause. Do not miss the practical recommendations, common misconceptions and summarizing key takeaways that will provide you with the necessary knowledge and skills in your clinical practice.
Join now!
This activity is supported by unrestricted financial support from Biocodex.
Who is Alessandra Graziottin?
Alessandra Graziottin, MD is an Italian gynecologist, oncologist, sexologist, and psychotherapist. She is the director of the Center for Gynecology and Medical Sexology at the San Raffaele Resnati Hospital in Milan.
- In 2008 she founded the Alessandra Graziottin Foundation for the treatment of pain in women Onlus, of which she is president.
- She is currently Consultant Professor at the Advanced Master in Andrology and Sexual Medicine of the University of Firenze.
- She also was Consultant Professor at the Advanced master's in clinical Sexology of the University of Pisa, and Professor at the Master Course of Sexual Medicine for Students of Psychology of the University of Venezia and Salesian University (UPS) of Roma.
She is a renowned gynecologist, having published 22 scientific books and 7 popular books (as the author, co-author, or editor), over 90 chapters of scientific books, 8 educational manuals for women, and more than 400 scientific articles on various aspects of gynecology and medical sexology.
Conflicts of Interest Statement: The author declares receiving honoraria from stellas, Fagron, Mammowave, Mylan, Named, Techdow, Uriach; participating as speaker in bureaus sponsored by Astellas, Biofemme, Bromatech, Lolipharma, Named, Techdow, Uriach; and being part of advisory boards of Astellas, Mylan, Techdow, Uriach.
What is Xpeer?
Xpeer Medical Education is the first accredited medical education app in the market, with video microlearning engaging videos of just 5 minutes.
With a powerful algorithm to personalize the user experience and the contents as the most popular entertaining streaming platforms, it offers a brand new experience for the continuing education and professional development of the healthcare professionals.
Accredited by the European Union of Medical Specialists, it delivers high quality scientific medical education pieces. On Xpeer, you will find this curriculum on Microbiota and 500 hours of medical education in 2021 in your specialty, technologies and professional and personal skills.
Information on accreditation
The app Xpeer is accredited by the European Accreditation Council for Continuing Medical Education (EACCME) to provide official ECMEC credits recognized officially in 26 countries.
The credits for the users of the module will be 1 European CME credit (ECMEC®) for every hour (60 minutes of actual e-learning excluding introductions etc.) of use, provided that the users have completed a module and have passed the relevant assessment.