Gastrointestinal motility and functional disorders
One of the highlights of this year’s event are numerous sessions dedicated to GI motility, with a main focus on functional diseases. In the opening ceremony, an update on refractory gastroesophageal reflux disease (GERD) was presented as a presidential lecture from Prof Somchai Leelakusolvong, President of Local Organizing Committee. Prof Somchai emphasized the importance of the Lyon consensus version 2.0, which has expanded the criteria of endoscopic findings to include Los Angeles reflux esophagitis grade B, which is more practical in Asian countries. The event also introduced many updated data on optimizing the treatment of refractory GERD based on various mechanisms. The advancements in treatment strategies were also highlighted, including the use of drugs targeting lower esophageal sphincter (LES) pressure, esophageal contractions, endoscopic interventions, and electrical stimulation. Transient lower esophageal sphincter relaxations were considered as one of the key mechanisms of GERD. This condition can be improved by baclofen by increasing resting LES pressure, thus reducing episodes of reflux. Preliminary data on a small cohort of patients suggested that electric stimulation could improve LES pressure; however, the practical application of this intervention in the future is still debated.
The event also paid considerable attention to the comparison between proton pump inhibitors (PPI) and potassium‐competitive acid blockers (PCAB) in different studies, with the target population being patients with erosive esophagitis. Current evidence showed a higher efficacy of PCAB compared to PPI in treating severe erosive esophagitis with acceptable adverse events.
One of the most engaging sessions was “All about GERD”, chaired by Prof Somchai Leelakusolvong and Prof Kwang-Jae Lee on December 8th. This session primarily focused on the updates of the modern Lyon consensus, non-acid reflux management, and optimizing treatment of functional heartburn.
Dr. Ping-Huei Tseng, Taiwan, presented the detailed changes of the Lyon consensus 2.0 with the clarification on the expanded criteria in endoscopic findings for Los Angeles grade B esophagitis. The role of high-resolution manometry to exclude mimic esophageal disorders and identify risk factors of GERD such as low LES pressure, hiatal hernia, or weak oesophageal contraction was also explained with case examples for further clarity. Some promising metrics on 24-hour pH impedance, such as mean nocturnal baseline impedance (MNBI) and post-reflux swallow-induced peristalsis (PPSW) index, are still debating and require further clinical data.
For non-acid reflux management, Prof. Justin Wu from Hong Kong highlighted the differences between the definition of refractory GERD and refractory GERD symptoms, of which the latter can be caused by various diseases. The roles of high-resolution manometry (HRM), endoscopy, and 24-hour pH impedance in the diagnosis and management of these conditions are explained in detail by the ESNM/ASNM guideline. The decision to perform 24-hour pH impedance on or off PPI depends on the diagnostic aim, whether to confirm GERD in patients with no prior diagnosis, or to confirm refractory GERD. It will be helpful to have a stepwise strategy for patients with refractory GERD to determine the optimal time for endoscopic interventions or surgery. Non-acid reflux management should be considered comprehensively for possible mechanisms, including characteristics of reflux episodes, oesophageal motility patterns, and overlapping symptoms. Furthermore, Prof Wu emphasized the need to establish a cut-off value for acid exposure time (AET) in GERD diagnosis for the Asian population, which can be a debating point when compared to the Lyon consensus.
Functional heartburn is also a challenging condition due to several factors: overlapping with other functional gastrointestinal disorders, presenting with mental disorders (anxiety, depression, stress) in the scope of the “gut-brain pathway” mechanism, and requiring exploration tests for exclusion. According to recent data, 70% of patients with functional symptoms had normal endoscopic findings. Within this population, 50% had normal 24-hour pH impedance results, and 60% showed no correlation with the occurrence of symptoms, meaning only 21% was classified as functional heartburn. That is why, besides PPI, neuromodulators play an essential role. Tricyclic antidepressants (TCAs) and selective serotonin uptake inhibitors (SSRIs) have shown efficacy in treating functional heartburn. However, their potential side effects should be carefully considered. For prevention, it is recommended to initiate treatment with a low dose and maintain follow-up during treatment.
Artificial intelligence in Endoscopy: ASPDE – WEO Symposium Highlight
Artificial intelligence (AI) is also a hot topic with many invited speakers. On the final day of APDW, December 9th, ASPDE cohosted with WEO to organize a session called “ASPDE-WEO International Clinical Symposium Artificial Intelligence in Endoscopy: Implementation in the Asia Pacific and the World”. This session was moderated by Prof Hisao Tajiri, Prof Yuichi Mori, and Assoc. Prof Nonthalee Pausawasdi. Prof Yuichi Mori gave the first presentation to introduce the WEO AI committee to the two ongoing projects. One project is an international study aimed at evaluating the perceptions of endoscopists and patients regarding the use of AI in endoscopy. The other is a longitudinal study on the role of AI in real-world settings. The WEO AI committee focuses on implementing AI in clinical practice, considering different aspects including accuracy, cost-effectiveness, doctor-machine interactions, training programs, and ethical considerations.
Prof Han-Mo Chiu, Prof Rungsun Rerknimitr, and Prof Kherk-Yu (Lawrence) Ho each presented different topics on developing and using AI effectively in several fields, including colorectal cancer screening, gastric cancer screening, and biliary endoscopy. The presentations showed many updated data, inspiring clinicians and endoscopists to consider implementing AI in the near future.
Assoc. Prof Dao Viet Hang presented another aspect of utilizing AI in endoscopy training, especially in limited-resources settings. She highlighted that the conventional metrics in endoscopy training, based on the minimum number of cases or the duration of practice, do not reflect the skills and personal development over time, requiring a more interactive approach. E-learning training programs and simulation-integrated activities have shown promising results in enhancing junior endoscopists’ knowledge and lesion detection skills. Until now, AI has shown promising data on improving lesion detection with more and more data in clinical practice; however, its integration in endoscopy training is still lacking. Some key considerations for applying AI in endoscopy training include economic feasibility, safety and accountability, technical concerns and validation, and clinicians’ role in digitalization. The framework suggested that adopting AI in endoscopy training should balance users’ factors, technology factors, social factors, and contextual factors (educational environment and standards). A needs assessment is required to outline educational needs and establish clear educational goals to inform Al’s technology selection. Al should be integrated into training based on the best evidence and within a curriculum, incorporating user training for both trainees and trainers to promote uptake.
All the talks in this session received substantial feedback, comments, and questions, reflecting a great interest in the future application of AI in endoscopy.
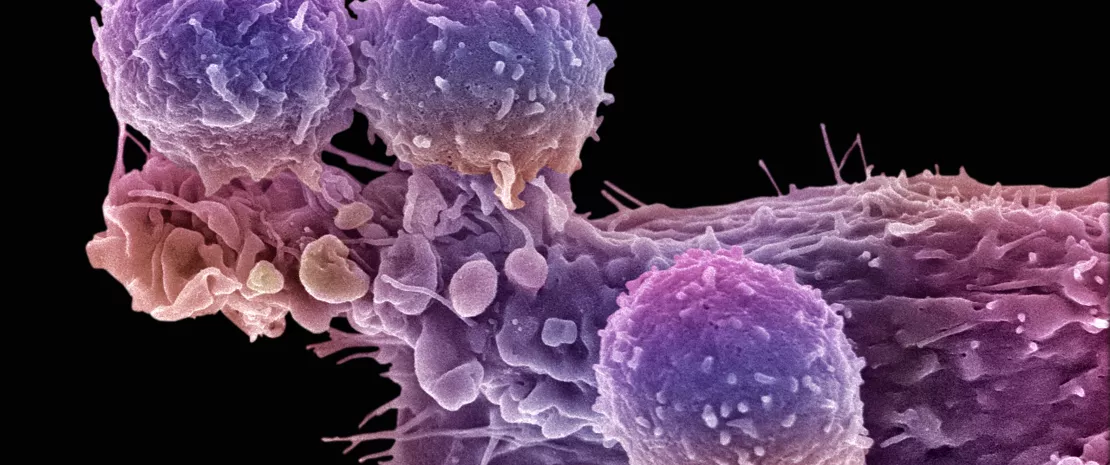
 Antibiotics disrupt cancer immunotherapy via gut and immune effects
Antibiotics disrupt cancer immunotherapy via gut and immune effects
 Pancreatic cancer: non-invasive early diagnosis thanks to the fecal microbiota?
Pancreatic cancer: non-invasive early diagnosis thanks to the fecal microbiota?