Despite widespread consensus that discrimination is a risk factor for mental and physical disorders, the exact mechanisms remain unclear. The hypothalamic-pituitary-adrenal axis has often been cited. However, some experts have now turned their attention to the gut microbiota in light of its extreme sensitivity to stressors, its role in inflammation and long-term health, and recent results with the gut-brain axis. A study published in 2022 investigated the effects of discrimination on dysregulation of the gut-brain axis.
Brain rewiring
Of the 154 participants in this study, 80 had experienced high levels of discrimination and 74 had experienced low levels of discrimination based on the color of their skin (African-American, Hispanic and Asian individuals), sex or age (Caucasians). High levels of discrimination went hand in hand with higher levels of anxiety, depression, and visceral sensitivity. However, the associations varied by ethnicity, with African-American individuals showing no association between discrimination and mental health, for example.
Physiologically, MRI results found that discrimination was associated with variable changes in stress brain connectivity pathways, depending on ethnicity: for example, in Asian individuals, discrimination was associated with higher stimulation of areas of the brain engaged in interoceptive, autonomic, sensory, motor, and reward processing, whereas Caucasian participants displayed a “chaotic” connectivity in numerous brain networks, etc.
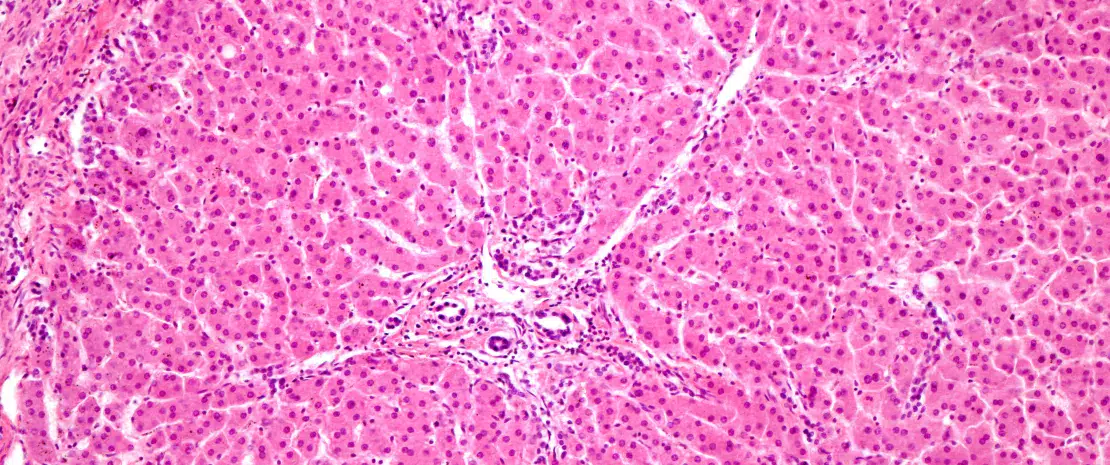
Dysbiosis of the gut microbiota
As well as these changes in the brain, discrimination also appears to be associated with gut dysbiosis and higher levels of the proinflammatory bacterium Prevotella copri among African-American and Hispanic individuals compared to Caucasian subjects. Bacterial metabolites were also affected, again with group-based variations: lower concentrations of a by-product of carnitine synthesis (an anti-inflammatory) among African-Americans; increase in metabolites involved in lipid metabolism among Asians, etc.
Discrimination with ethnicity-mediated consequences ?
The authors believe that discrimination affects the gut-brain axis, with consequences that vary between communities.
- Among African-Americans, there is a stronger association with inflammatory biomarkers, but this group appears less prone to anxiety and reports the highest resilience scores.
- Among Hispanics, discrimination is also associated with inflammation, but this group has better coping strategies.
- The results for Asians suggest they deal with stress by a diet high in fat.
- For Caucasians, the observed brain changes could indicate coping difficulties.

 After all, eating Big Brother's snot might not be a bad idea
After all, eating Big Brother's snot might not be a bad idea