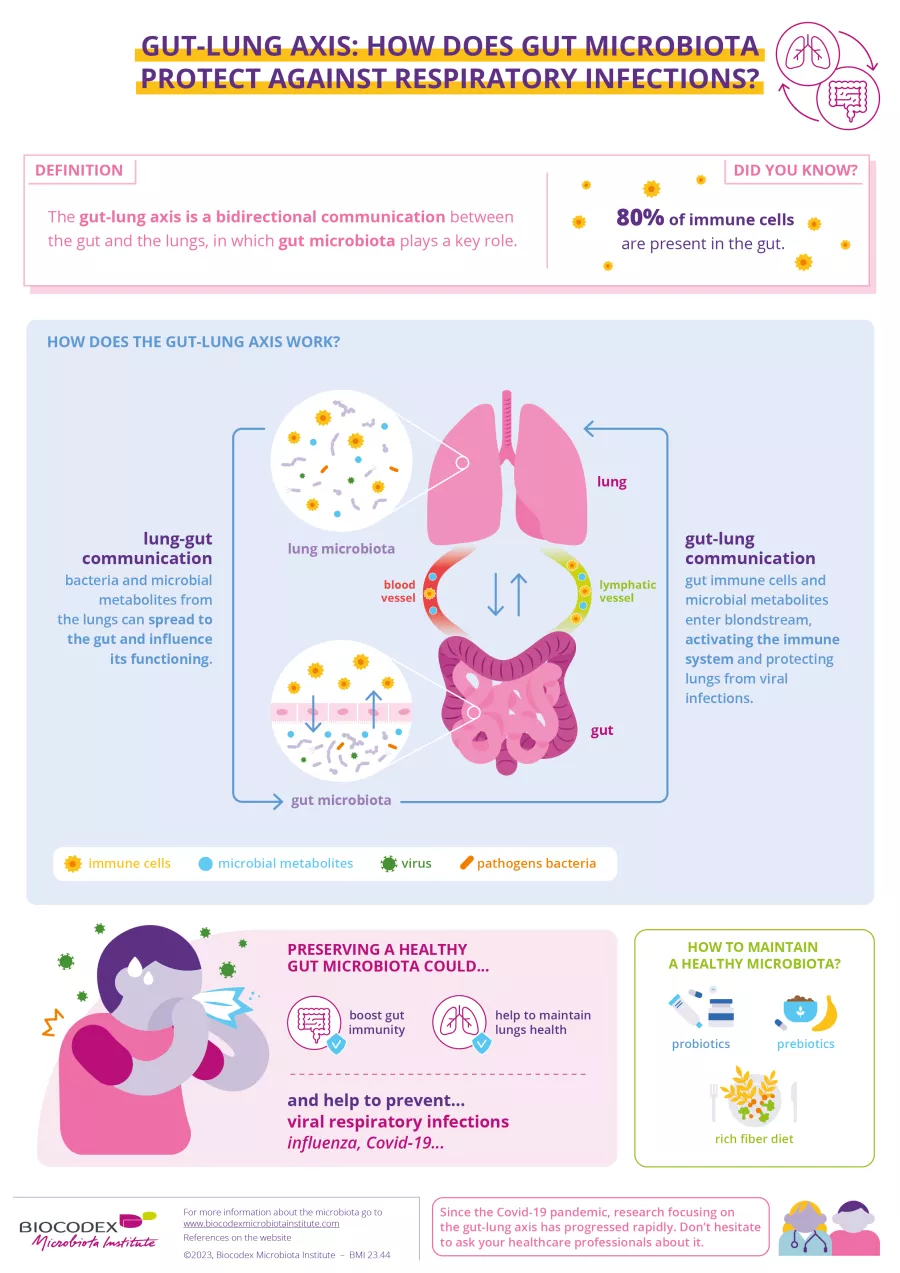
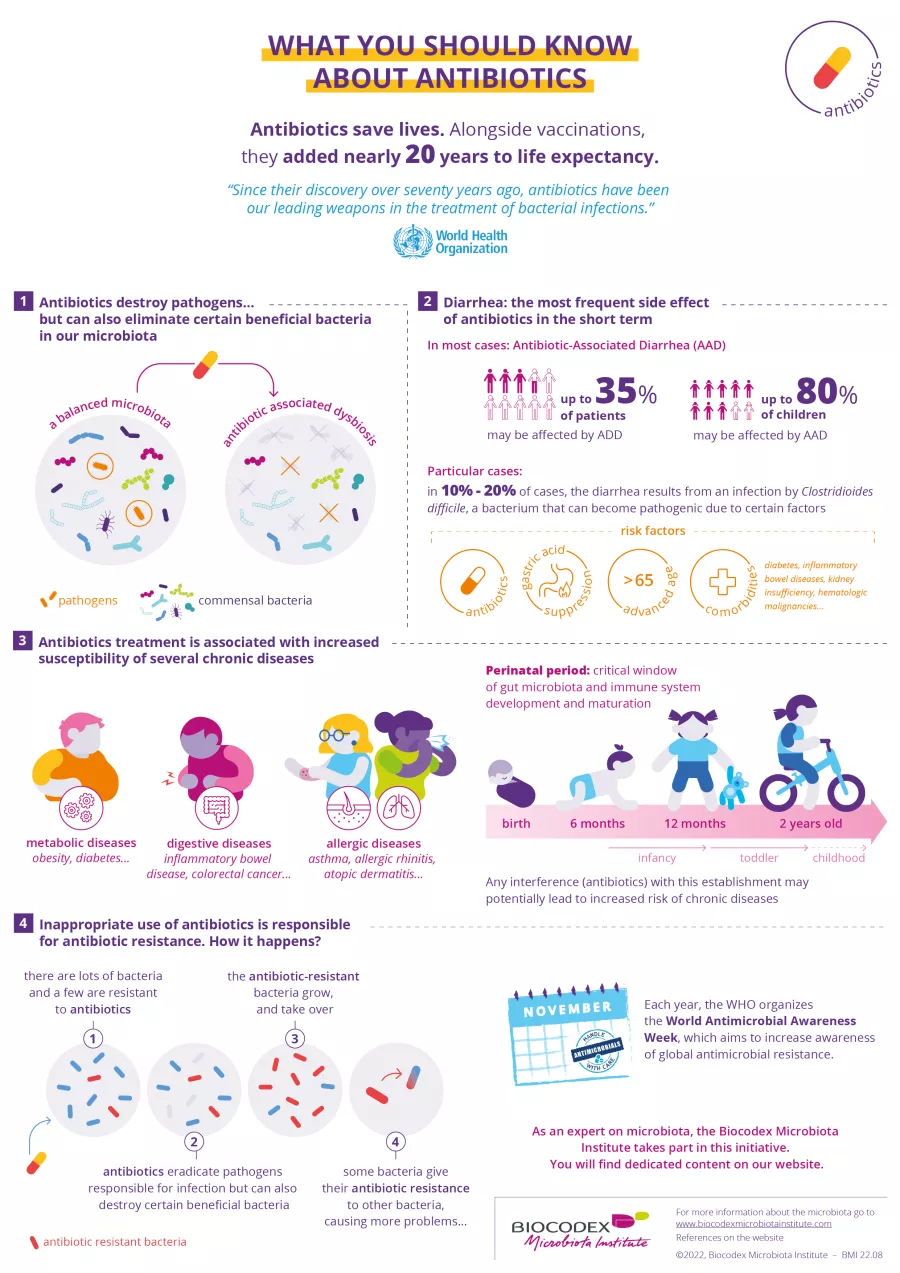
The tightly regulated interplay between gut microbiota and host influences many physiological functions including immune homeostasis. A body of preclinical and clinical evidence shows that gut microbiota composition is transiently altered in the context of acute viral respiratory infections. In the case of Covid-19, studying the gut microbiota during infection is particularly important, given that SARS-CoV-2 can bind to ACE2 receptors in the gut, the virus is found in the intestine in up to 25% of patients, and the gut microbiota alterations associated with pulmonary and intestinal complications are likely to influence disease severity. This preclinical study is the first to investigate the role of SARS-CoV-2 infection in dynamic changes in the gut microbiota of monkeys.
The monkey: a good model for SARS-CoV-2 infection
The human data currently available on Covid-19 are abundant but do not allow the disease to be followed throughout its course, from pre-infection to post-resolution. The researchers used two species of monkeys (cynomolgus monkey and rhesus monkey) to fill in certain missing pieces of the infection puzzle. These non-human primates are a suitable model for the study of Covid-19, since SARS-CoV-2 infection led to virus replication in their upper and lower respiratory tracts, resulting in lung pathology and respiratory disease with no overt clinical symptoms. Two monkeys from each species were infected intranasally and intratracheally. Blood (to measure cytokine levels) and stool samples were collected 9 days prior to infection and at 0, 3, 5, 7, 10, 13, 20, and 26 days post-infection (dpi). Two of the monkeys had transient diarrhea at 4 dpi.
Covid-19: persistent dysbiosis even after resolution...
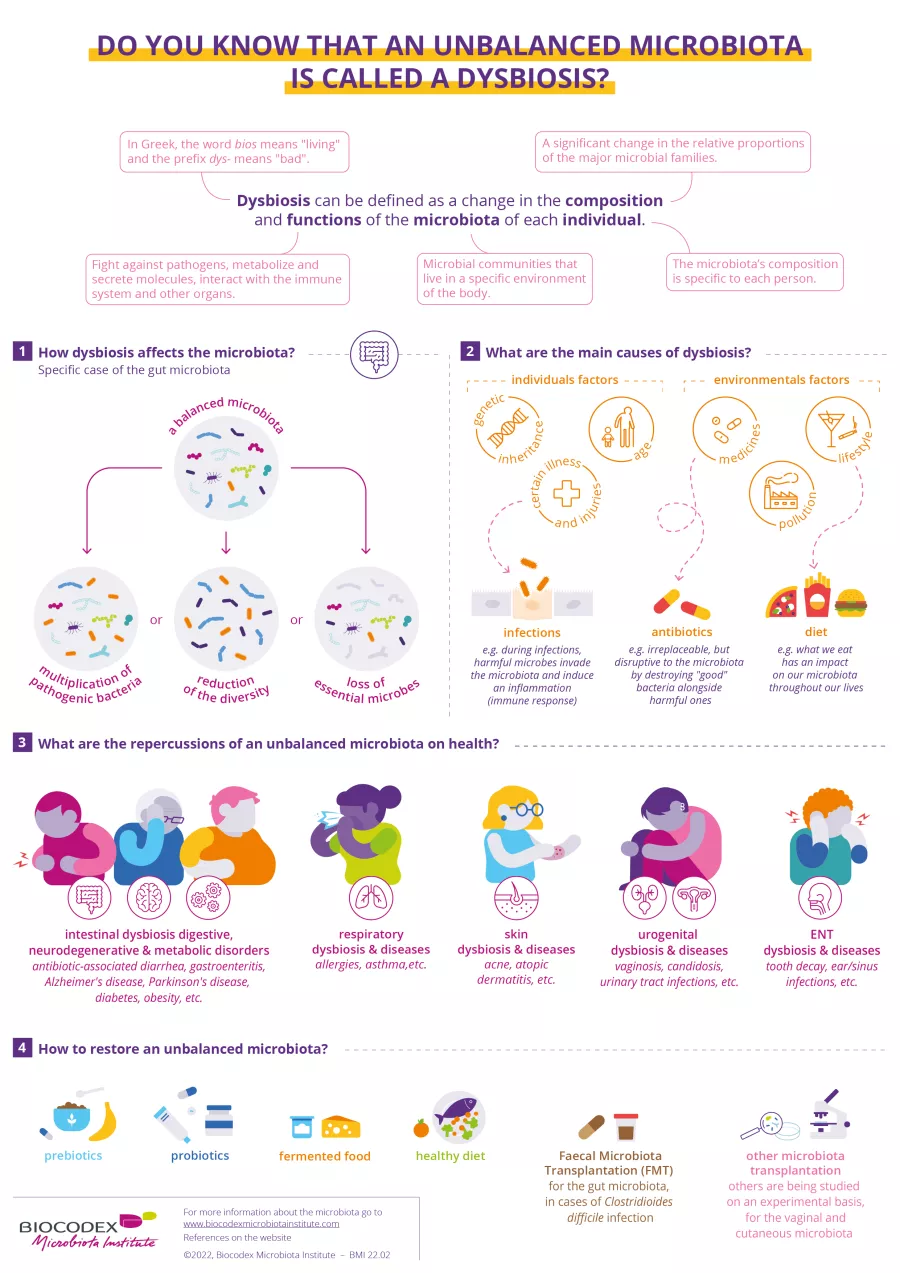
16S rRNA gene sequencing revealed significant changes in the composition of the monkeys’ gut microbiota, with a peak at 10-13 dpi. Some alterations in the microbiota persisted after SARS-CoV-2 was eliminated from the upper respiratory tract (virus undetectable in the nasopharynx and trachea at 20 dpi, but still detectable in the stool of two monkeys) and even at 26 dpi. A significant number of changes in the abundance of bacterial taxa were observed during infection, particularly at 13 dpi. In particular, the relative abundance of Acinetobacter and some genera of the Ruminococcaceae family was positively correlated with the presence of SARS-CoV-2 in the upper respiratory tract.
...and a gut microbiota with altered functional activity
A metabolomic approach was used to evaluate the functional consequences of the changes in the gut microbiota associated with the infection. The aim here was to quantify three of the most important categories of microbiota-derived metabolites: short-chain fatty acids (SCFAs), bile acids, and tryptophan metabolites. SCFA levels changed over the course of the infection, particularly between 2 and 13 dpi. Changes in several bile acids and tryptophan metabolites were also identified in infected animals. The relative abundance of several taxa known to be SCFA producers (mostly from the Ruminococcaceae family) was negatively correlated with certain systemic inflammatory markers, while the genus Streptococcus was strongly and positively correlated with the same markers. This study shows that experimental infection with SARS-CoV-2 in monkeys is associated with a disruption of the gut microbiota’s composition and functional activity. The persistence of dysbiosis after resolution of the infection may play a role in the long Covid-19 symptoms currently being reported in humans.