My name is Jennifer, I’m 32 years old and I work as a product manager in the fashion industry.
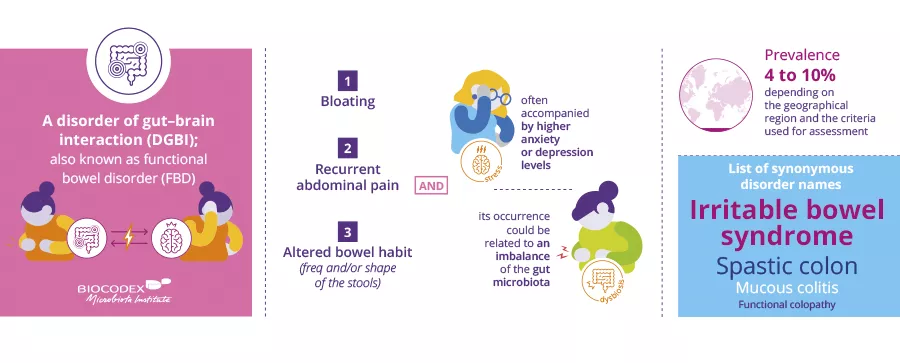
Can you explain what is irritable bowel syndrome?
Irritable bowel syndrome is a chronic, invisible, and misunderstood digestive disorder.
What were your symptoms?
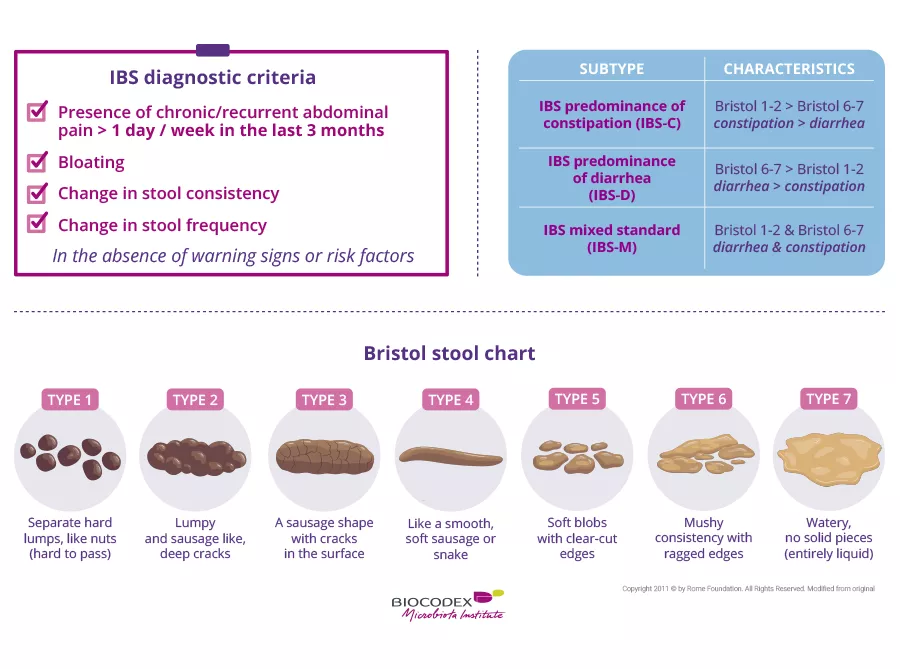
I had constipation that felt like daggers in my stomach, pain, spasms, nausea, and occasionally diarrhea. I also suffered from chronic fatigue.
My first symptoms, surprisingly, were food allergies, while I also developed Raynaud’s syndrome, where blood no longer circulates to extremities (hands and feet), leaving them extremely cold.
I had back pain that forced me to wear a corset belt at the age of 25.
How long did it take to get diagnosed?
I had these symptoms for 21 years before being diagnosed at the age of 29.
What made you seek medical advice?
I woke up one morning still extremely tired and very late for work. And I suddenly collapsed.
Where did you look for advice about your symptoms?
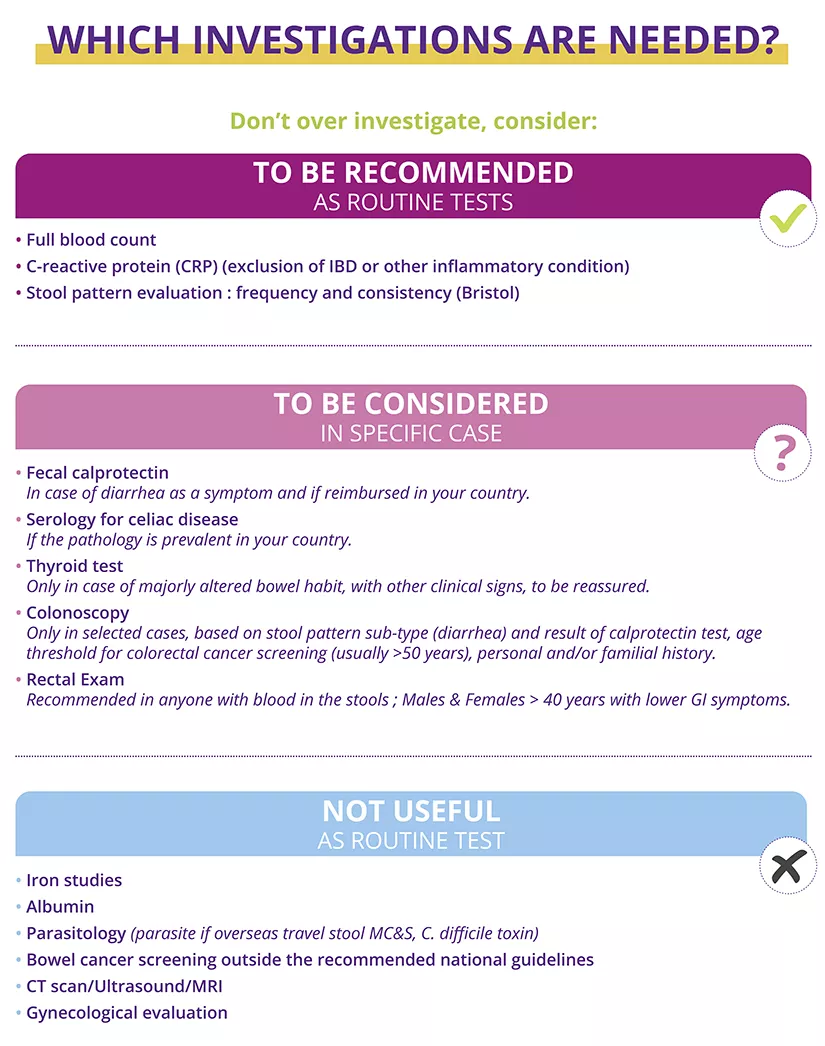
At first, I sought advice from my family doctors and gastroenterologists, but the answers were always the same: since I had been acutely constipated at the outset, they prescribed me lots of laxatives and didn’t look into it any further. I also saw rheumatologists but got no real answer until the last gastroenterologist told me about IBS and FODMAPs.
What are FODMAPs?
FODMAPs are fermentable sugars in food. For people affected by IBS, they can be a problem.
Did you know that the gut microbiota may be involved in IBS?
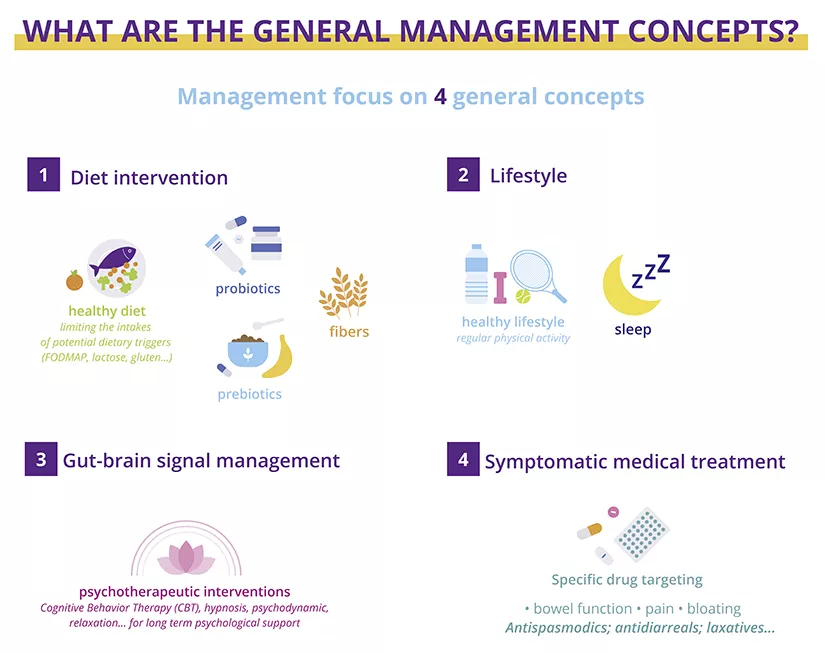
I knew my microbiota was involved as soon as the gastroenterologist told me that my diet was part of the problem. As soon as I changed to a low-FODMAP diet that replenished my microbiota, literally all my symptoms disappeared.
What’s it like living with IBS on a daily basis?
I manage the illness on a daily basis by maintaining a healthy lifestyle. I make sure to sleep well, I’m careful about what I eat, and I try to avoid as best I can any unnecessary stress that could affect my stomach and, therefore, my head.
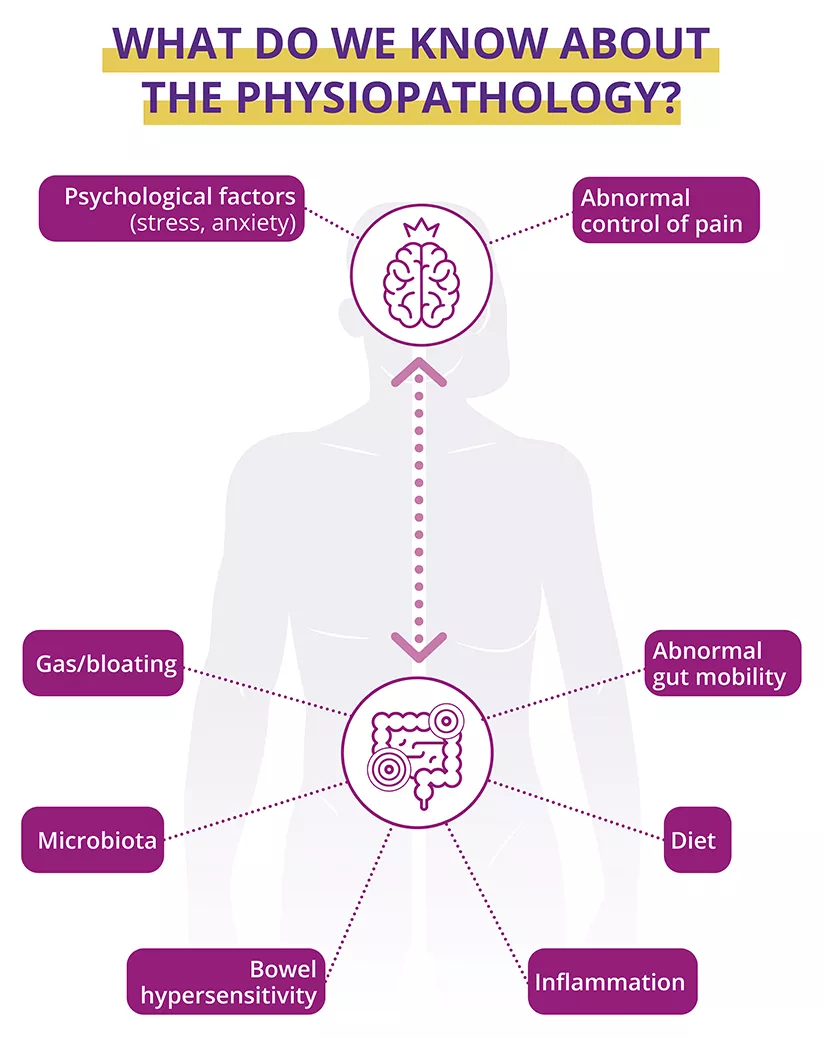
What do you know about the gut-brain link in IBS?
I think IBS shows that the head and stomach are intricately linked. For me, the gut is even a precursor to the brain. When things go wrong in the stomach, they’re bound to go wrong in the head.
What message do you have for people with IBS?
I’ve so much advice for people with IBS that I’ve created a blog called foodmapers.com where you can find everything I have to share.
Listen to your own body, trust yourself. It’s not in your head. If you feel there’s something wrong, it may be due to your microbiota and the way you digest food.
I’ve been there. You can’t go on having x-rays and ultrasounds for another twenty years only to be told there’s nothing wrong. There must be something going on. And once it’s been diagnosed, there are plenty of things you can act on in terms of diet, stress and anxiety, and sleep.
In conclusion
Stay positive, but above all keep searching, don’t give up, and find health professionals who can support you and help find what’s wrong.

 Inflammatory Bowel Disease (IBD): do microplastics condition severity?
Inflammatory Bowel Disease (IBD): do microplastics condition severity?
 Everything you need to know about Dysbiosis
Everything you need to know about Dysbiosis