Is there a key to understand vulvar and sexual pain?
Vulva, vagina, labia: what are the differences?
Keys to a successful consultation by Alessandra Graziottin
Beyond diversity: unveiling the secrets of a healthy gut microbiome
The conventional view of a healthy gut has long been dominated by the idea that diversity is king. A high variety of microbial species was thought to be the primary indicator of a well-functioning gut. However, our sources suggest that this is far too simplistic. So what makes a “healthy microbiome”?
The gut microbiota Prebiotics: what you need to know Digestive disorders Diet
The antidepressant effect of citrus: a matter of gut bacteria?
Consumption of citrus fruits could reduce the risk of depression by 22% via the gut-brain axis. Flavonoids in citrus fruits are thought to promote beneficial bacteria, such as Faecalibacterium prausnitzii, which produce a metabolite that improves the availability of serotonin and dopamine.

 Gut microbiota: a common signature for psychiatric disorders?
Gut microbiota: a common signature for psychiatric disorders?
 Premenopause and depression: towards a new management pathway?
Premenopause and depression: towards a new management pathway?
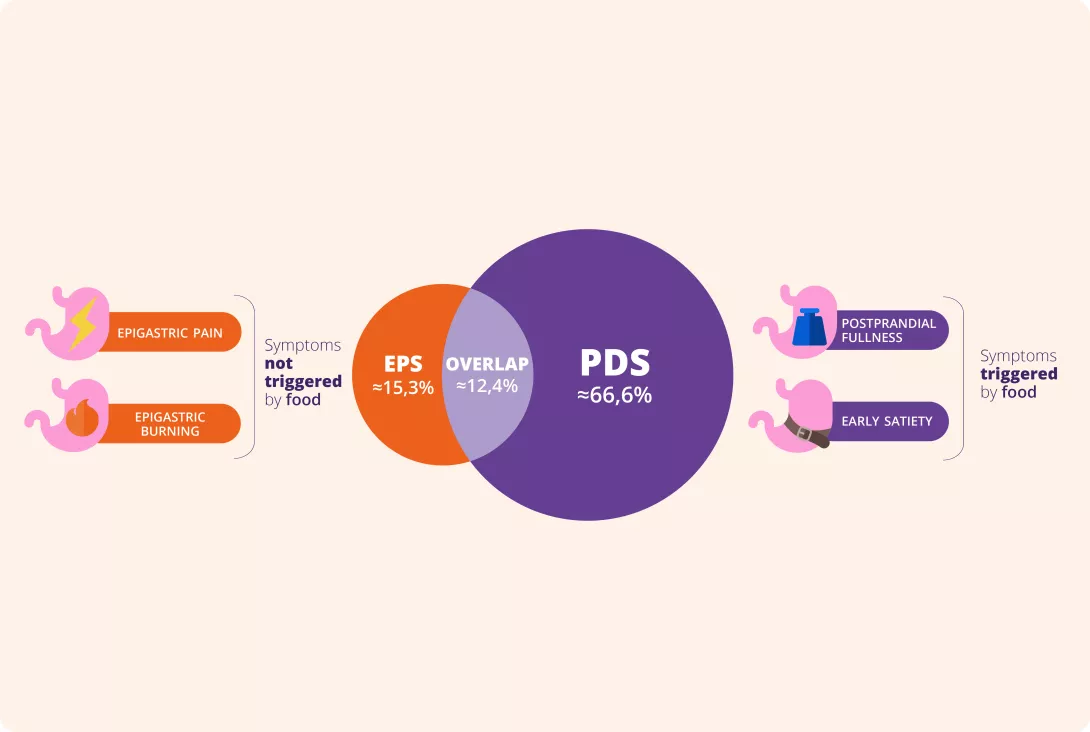
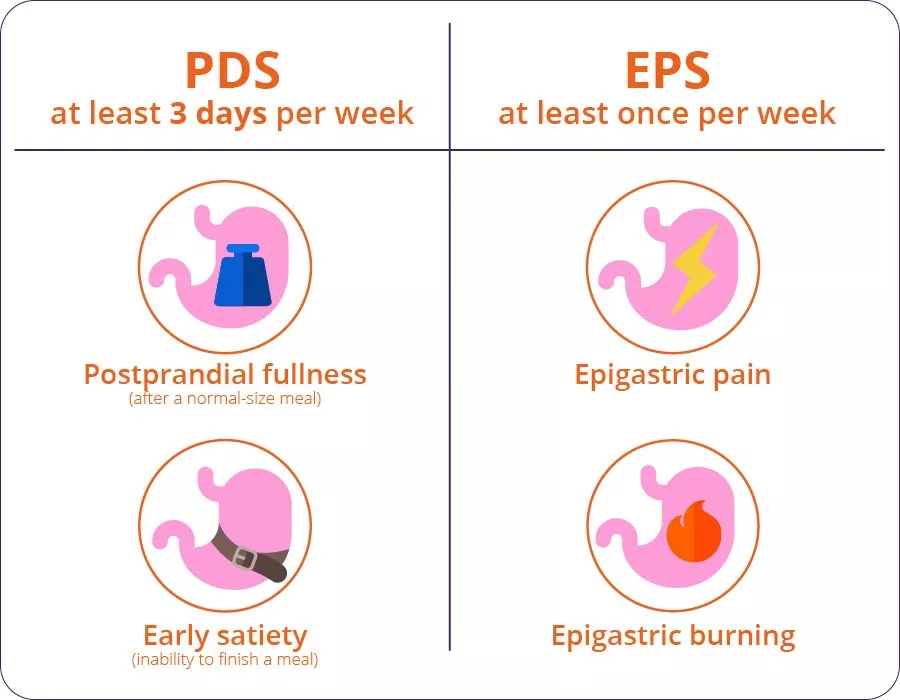
Your functional dyspepsia diagnosis check list
How many patients with persistent upper gastrointestinal discomfort do you see each week? How many remain undiagnosed with Functional Dyspepsia (FD)?
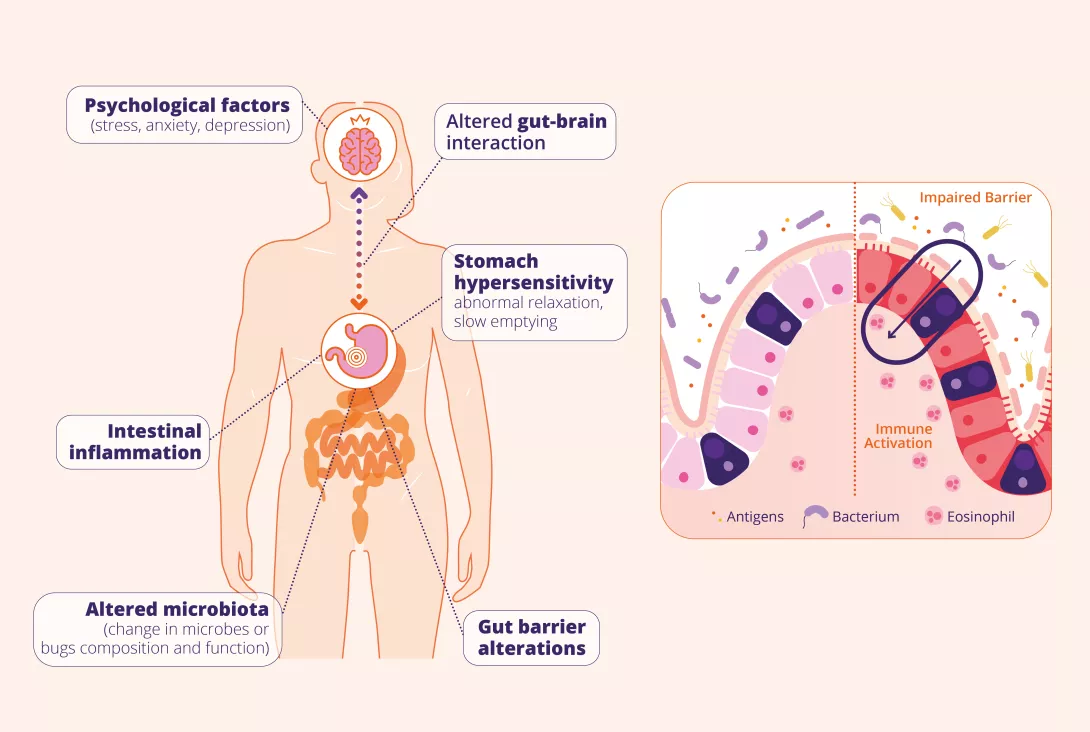
FD affects about 7% of adults3 but is often misdiagnosed due to overlapping symptoms with reflux, gastroparesis, and IBS. As a disorder of gut-brain interaction, it involves altered motility, microbiota imbalances, and psychological factors, making diagnosis challenging.
To help, Prof. Maura Corsetti, Prof. Nicholas Talley, and Prof. Lucas Wauters, in collaboration with the Biocodex Microbiota Institute, have developed a Functional Dyspepsia Diagnosis Checklist. This tool aids in more accurate diagnosis and clearer patient communication, improving management and care.
Citrus and bacteria: a natural cocktail to counter depression
Eating citrus fruit could reduce the risk of depression by 22%. The flavonoids present in these fruits are thought to promote certain good gut bacteria, thereby increasing the availability of substances essential to our well-being, such as serotonin and dopamine.
The gut microbiota Psychiatric disorders Diet
 Why running could bring a smile to depressed teens... and their gut microbiota
Why running could bring a smile to depressed teens... and their gut microbiota
 Mental illness and the gut microbiota: the end of a riddle?
Mental illness and the gut microbiota: the end of a riddle?
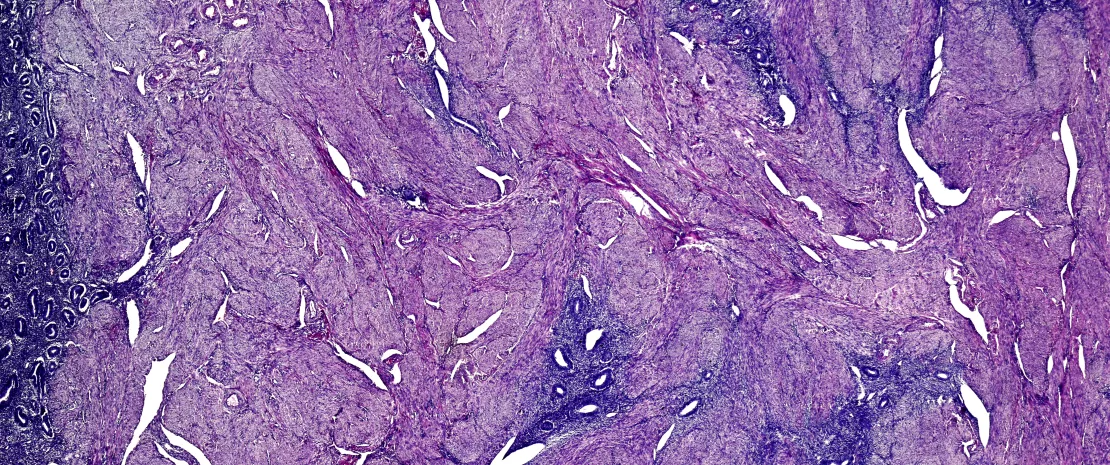
Towards a microbiotic marker for endometriosis?
The oral, gut, and vaginal microbiota of women suffering from endometriosis display specific characteristics. These bacterial signatures may one day serve as biomarkers for diagnosing the disease and its severity.
 Endometriosis: A key to its progression in the gut microbiota?
Endometriosis: A key to its progression in the gut microbiota?