The first thousand days : a crucial time for Microbiota
By Dr. Marta Ardila Jimenez
Coordinator, Pediatrics and Neonatalogy Department, Clínica de Marly Jorge Cavelier Gaviria, Bogota, Columbia
At the 56th congress of the ESPGHAN, in MIlan, Microbiota was one of the congress’ main protagonists, thanks to the increasing number of ascending studies and the imperative necessity to learn more about this topic every day. We are living in a new era in which microbiota plays a fundamental role in how we will fulfill our duty to reduce disease rates for future generations. But as fellow doctors, how can we teach this information to our patients in order to prevent constant disease?
When reflecting on how certain strategies could impact the evolution of the weight of disease carried by the general population, numerous research efforts have proven that the first 1,000 days of life are a critical time period that represents the opportunity to cause a positive intervention and prevent a lifetime of non-communicable diseases. Why is it so important? Well, this period is fundamental for intestinal colonization, and, subsequently, the establishment of microbiota. Hence, it has significant control over intestinal maturation and both metabolic and immunological programming. Microbial colonization of the gastrointestinal tract is fundamentally linked to metabolic programming, immunologic maturation any perturbations in colonization during infancy have been associated with increased risk for multiple conditions, including asthma, atopic dermatitis, food allergy, diabetes, inflammatory bowel disease, and obesity. 1
Since the beginning of the embryonic phase, both development and growth rates are determined not only by genetic load but also by the environmental factors to which a child is going to be exposed. Epigenetic mechanisms such as the modification of histones, non-codifying RNA, and DNA methylation are heavily impacted by these critical factors, such as the consumption of specific substances, certain diets, and large amounts of stress. Every stage of growth and development is crucial for determining the positive effects microbiota can have on a patient, just like a puzzle requiring all of its pieces to be complete.

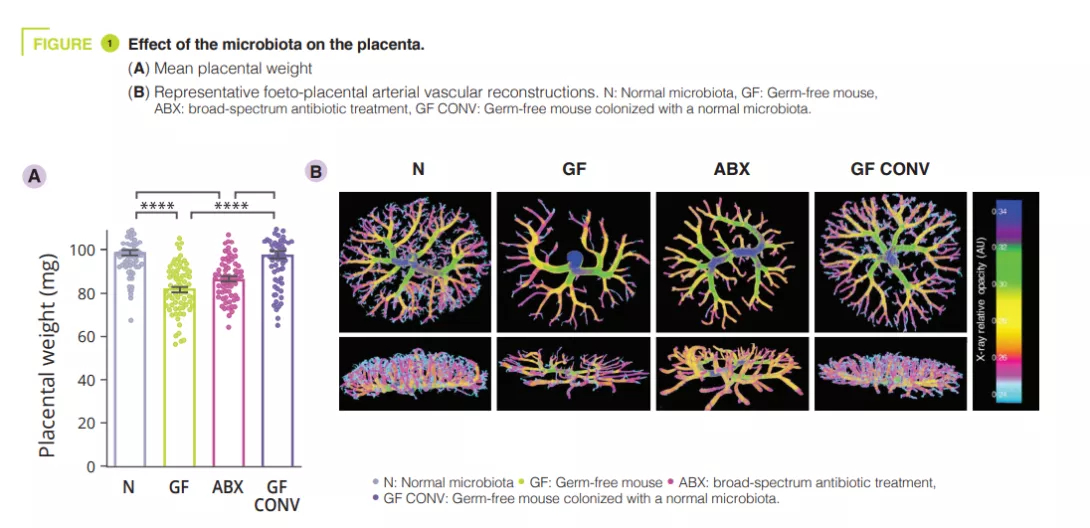
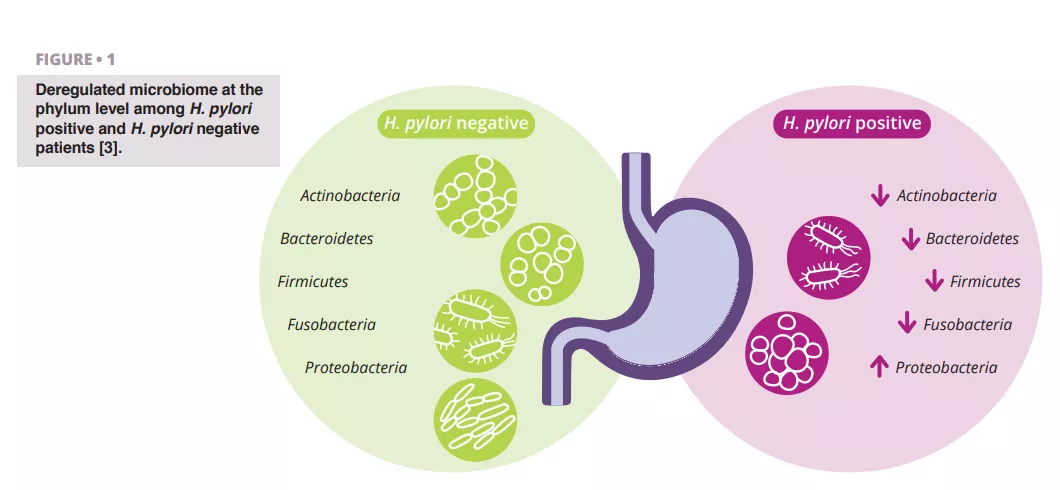
Studies carried out on microbiota during the gestation period show changes in a mother’s macrobiotic composition in varying body sites, including the endometrium, vagina, and gut, in some cases even causing pregnancy complications. As we go further along during the first trimester of pregnancy, the microbiota’s intestinal constitution is similar to the one of healthy, non-pregnant women 2. Throughout the third trimester microbiota’s diversity exponentially increases, causing some weight gain, insensibility to insulin, higher concentration of fecal cytokines , which is reflected by inflammation. There will also be higher levels of Bacteroides and Staphylococcus found in feces of overweight pregnant women as compared to those who sustain a healthy weight. The vertical transition of bacteria from a mother to a newborn contributes to the development of microbiota on the intestinal tract and can affect the function and growth of that specific immune system. Notable differences between the mother’s and newborn’s microbiota born by a natural birth or a c-section babies born through a natural process. Surprisingly, several studies show that children born through a c-section have a stronger chance to experience immune disorders such as allergies and asthma. It is at the very moment of the first skin to skin contact that breastfeeding plays a crucial role in enriching the newborn with several nutrients that will help preserve its immune system 3, 4.
The timing of introducing solid foods also influences gut microbiota composition. In preterm infants the gut microbiota development is influenced by multiple factors, including the time since birth and the intake of breast milk, and interventions such as probiotics and prebiotics supplementation show promising results in reducing morbidity and mortality in this population.
Having a clear understanding on how these first thousand days impact the newborn’s life as an adult, our mission will be to conduct public policies to strengthen microbiota. We can achieve this goal by taking action, from caring and nurturing a lactating mother, to incentivizing the practice of breastfeeding and most importantly reporting and communicating information about healthy nutritional habits to all of our patients.