The International Microbiota Observatory 2025 - Press release
Microbiota Momentum: Bridging Awareness and Action
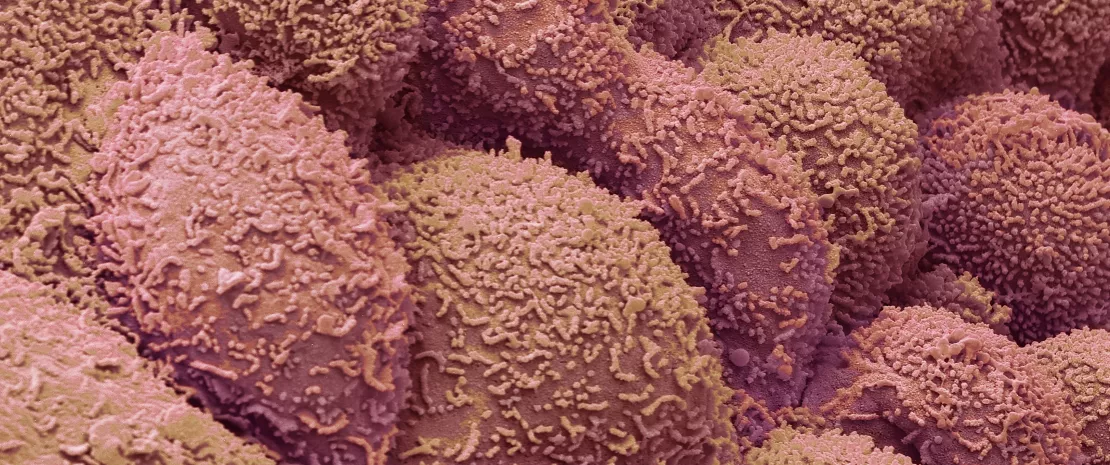
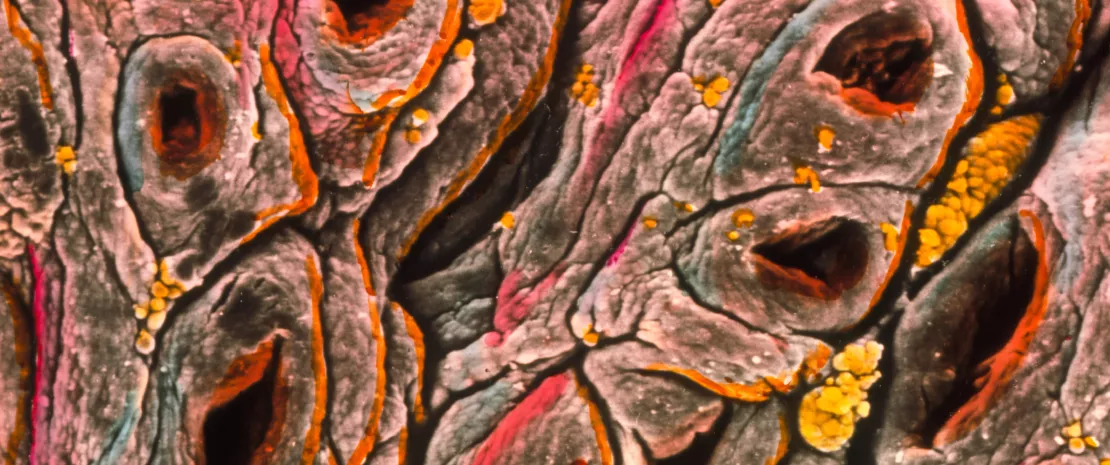
Microbiota is made up of trillions of microorganisms such as bacteria, viruses, fungi, archaea, etc. It lives in our digestive tract, our skin, our mouth, our nose and our lungs. These organisms play a crucial role in our wellbeing by helping digestion, stimulating our immune system, and protecting us from infectious diseases. But beyond these functions, microbiota also influences our mood, our metabolism and even our longevity. An imbalance of microbiota, often caused by factors such as diet, lifestyle or medication, could lead to major health problems, from digestive disorders to cardiovascular problems and depression. Maintaining a healthy microbiota throughout our bodies is therefore essentialfor our general health and well-being.
For the third year running, the Biocodex Microbiota Institute has commissioned Ipsos to conduct a major international survey on microbiota: the International Microbiota Observatory. What are the trends in microbiota awareness? Have individuals adopted more behaviors to protect and preserve their microbiota this year? What role do healthcare professionals play in educating their patients? What are people’s thoughts on microbiota testing?
This large survey was conducted by Ipsos among 7,500 people in 11 countries (the USA, Brazil, Mexico, France, Germany, Italy, Portugal, Poland, Finland, China and Vietnam). Within each country, a representative sample of the population aged 18 y.o. and over was interviewed. Representativeness was ensured by the quota method applied to the respondent’s gender, age, region and occupation. The survey was conducted online, from January 21 to February 28, 2025.
The results were presented on June 27, 2025, on the occasion of World Microbiome Day.
2025 results: The International Microbiota Observatory

“Awareness about the microbiota is just the beginning. Taking action to preserve its balance is the following step. This year, the Biocodex Microbiota Institute has taken a step further by turning data into action. In partnership with Le French Gut, we’re translating knowledge into public engagement — empowering citizens, researchers, and healthcare professionals to work hand-in-hand for better health.”
About the Biocodex Microbiota Institute
The Biocodex Microbiota Institute is an international hub of knowledge dedicated to microbiota. The Institute educates the lay public and healthcare professionals on the importance of microbiota in healthcare and well-being.
Press contact Biocodex Microbiota Institute
Olivier Valcke
Director of the Biocodex Microbiota Institute
Global Microbiota Communication
+33 6 43 61 32 58
o.valcke@biocodex.com
Press contact Ipsos
Etienne Mercier
Director of Opinion and Health – Ipsos Public Affairs
+33 6 23 05 05 17
Etienne.Mercier@ipsos.com