Towards a more favorable exposome
We still have a long way to go before we can understand and measure the impact of all environmental exposures on human health.

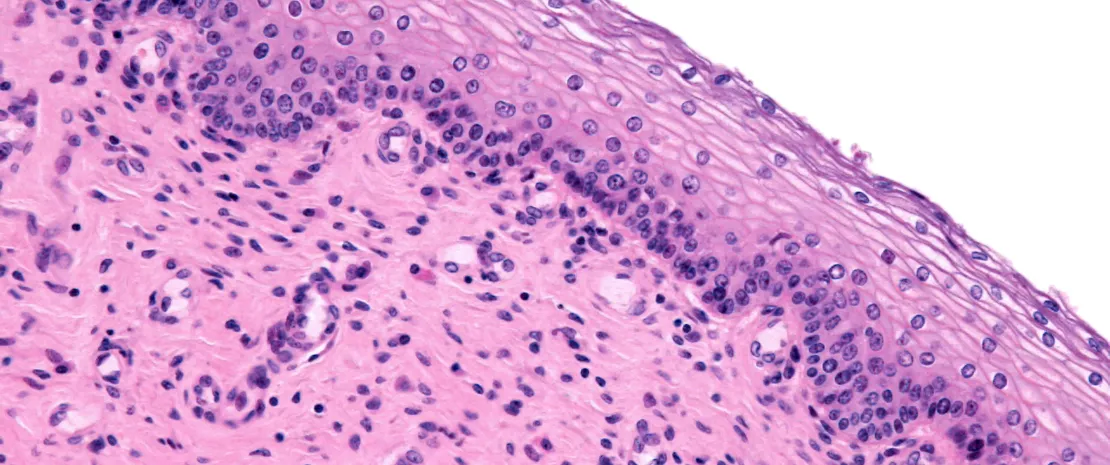
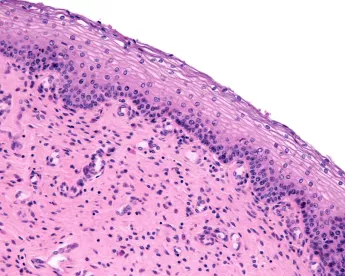
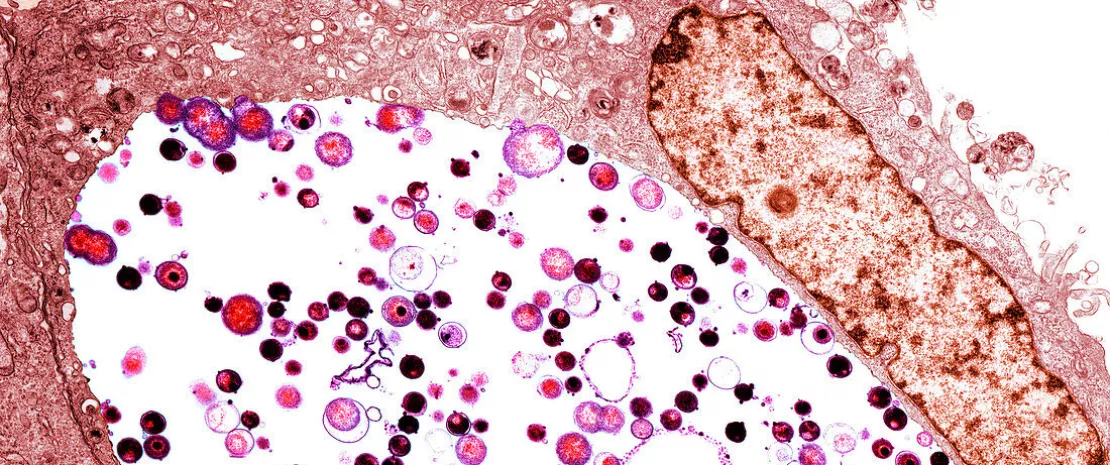
However, initial studies suggest that the microbiota, as the interface between our body and the outside world, may play a key role. They show that:
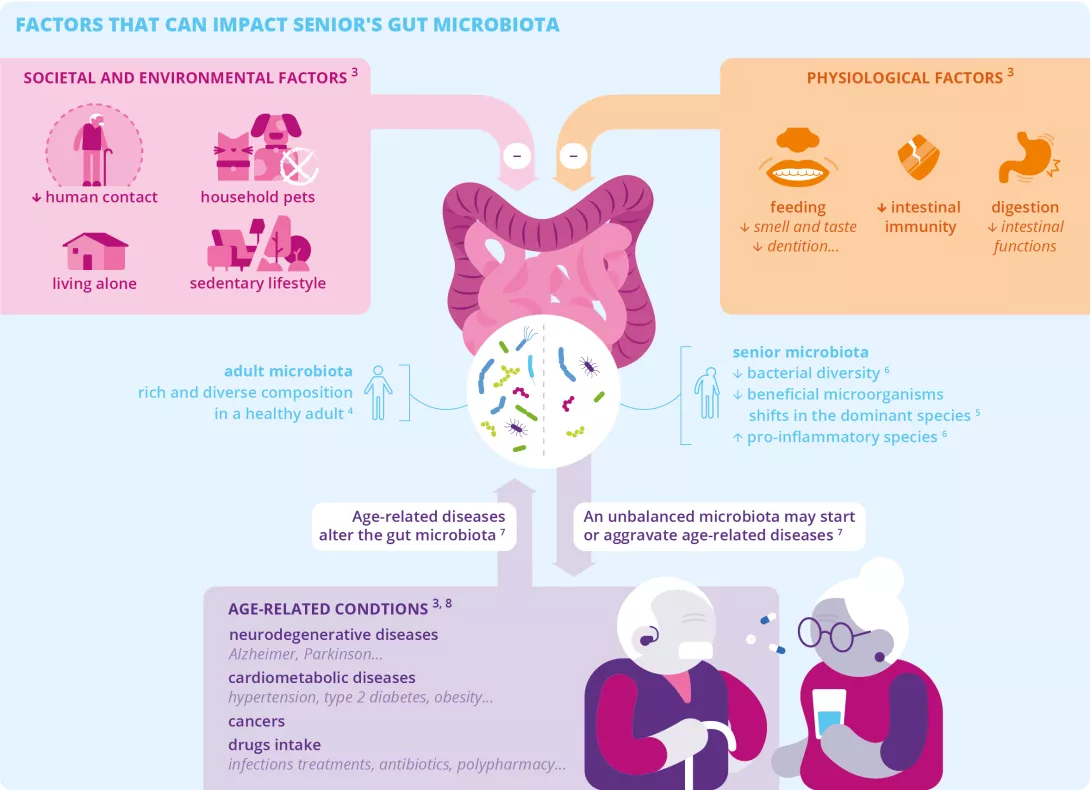
- Lifestyle modernization is having as much impact on ecosystems as on our health and the health of our microbiota;
- An environment rich in diverse microbes plays a protective role;
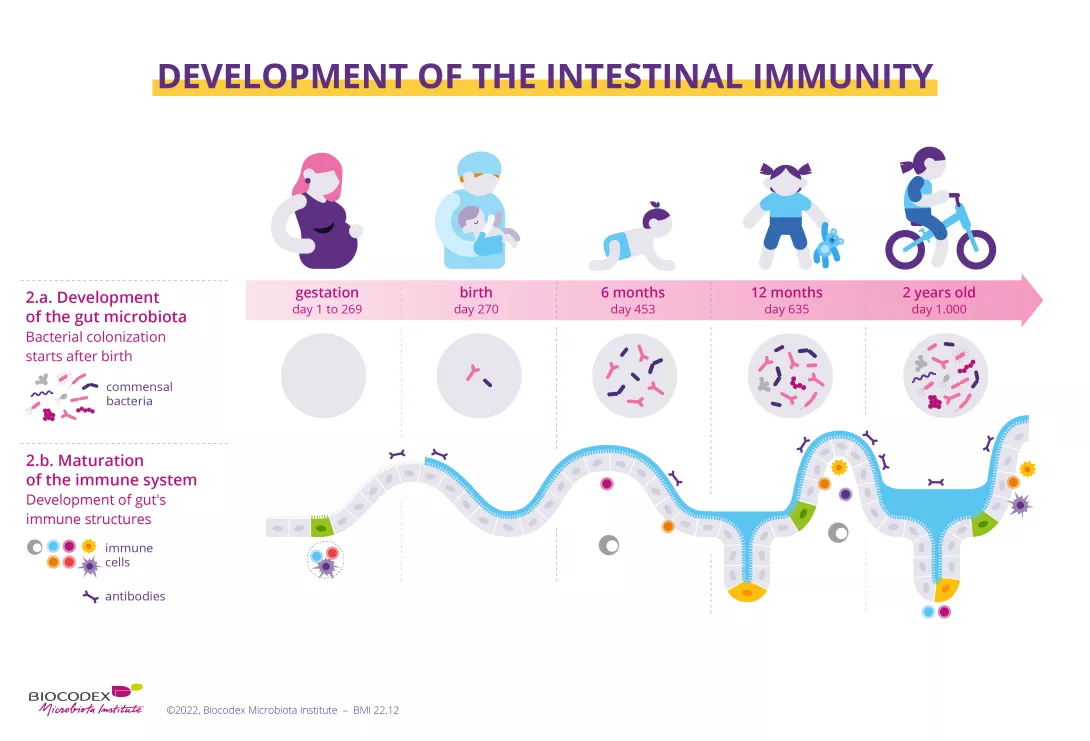
- At the very beginning of life, there’s a window of opportunity where the nature of exposures can predispose the body to chronic disease or, on the contrary, protect it;
- There are simple ways (low-processed and plant-based food, physical activity, quality sleep, contact with nature, limiting chemicals and drugs, etc.) to move towards an exposome more favorable to our health.
In practice
Even if we can’t control all the factors to which our bodies are exposed, a few simple behaviors and habits can help reduce harmful exposures and give more room to those that protect us.
Diet
- Favoring whole, organic, and seasonal foods (fruits, vegetables, legumes, wholegrain cereals, etc.), which are rich in fiber, vitamins, and minerals, and reducing our intake of ultra-processed foods (ready-made meals, processed meats, snacks, industrial cakes, sweets, etc.);
- Give preference to poultry and limit other meats (pork, beef, veal, mutton, lamb, offal) to 500 g per week; alternate with foods that provide more plant proteins, such as pulses or whole or semi-whole cereal products;
- Avoid bottled water, which likely contains microplastics; instead opt for water filtered with an activated carbon cartridge or reverse osmosis system, which at present appear to be the most effective means of eliminating “forever chemicals” (PFAS) 40;
- Limit the use of plastic packaging and stretch film, and instead use bulk packaging and bee wrap (cloth coated with beeswax) to cover leftovers and wrap snacks;
- Use glass or Pyrex (inert) containers instead of plastic containers, especially when heating food in the microwave;
Microplastics: beware of takeaway food packaging and their impact on the microbiota!
Hygiene
Use the most simple and unscented products available: vegetable oils, hydrolats, natural soaps, creams based on natural products with a limited number of ingredients, etc. Apps such as Yuka, INCI Beauty, and QuelProduit allow you to scan products and identify those that contain fewer problematic substances.
Health
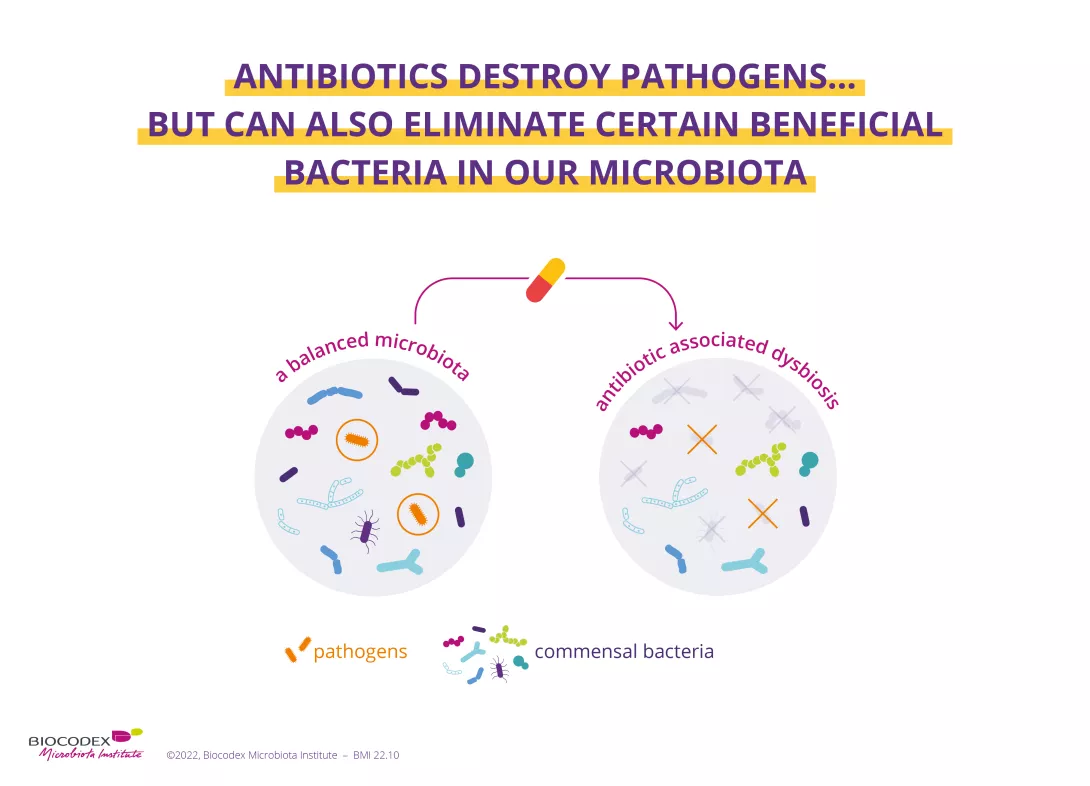
- Avoid self-medication, especially with antibiotics;
- Return unused medicines to the pharmacist (avoid throwing them in the garbage or down the sink);
Antibiotics: what impact on the microbiota and on our health?
Household
- For the household, use traditional products (Marseille soap, vinegar, soda crystals, clay powder, etc.) and avoid harsh, perfumed detergents and fabric softeners;
- Avoid going on a germ hunt by banning bleach and all anti-microbial products from your home;
- Avoid scented candles, air fresheners, sprays, etc.;
- Avoid particle board furniture, varnishes, paints, etc. – sources of volatile organic compounds (VOCs) – especially in babies’ and children’s bedrooms;
- Air rooms for 10 minutes a day.
My family, my roommates, my neighbors... and my microbiota
Leisure, physical activity, stress management
- Spend as much time as possible in contact with nature;
- Let children play in contact with vegetation and animals.
- Limit screen time and instead encourage artistic, creative, and shared leisure activities (games, music, painting, etc.).
- Avoid a sedentary lifestyle by making physical activity part of your daily routine: walk, cycle, or rollerblade instead of using motorized transport; take the stairs instead of the elevator, etc. ;
- Opt for environment-friendly vacations, whether in terms of practices or transport;
- Look after your mental health by practicing stress management techniques (meditation, breathing, cardiac coherence) and learning to slow down, listen to yourself, contemplate, communicate, etc.
Microbiota & sport: competitive micro-organisms
Professional activity
- Inform yourself about any occupational exposure to chemical substances (diesel emissions, silicon dioxide, asbestos, etc.), biological agents (bacteria, viruses, or molds likely to cause infection, allergy, or poisoning), physical agents (noise, heat, cold, radiation, etc.), and stress (working hours, work pace, lack of resources, interpersonal tensions, etc.);
- Follow professional preventive advice
Read another article
Get your microbiota ready to go back to work
Back to previous page
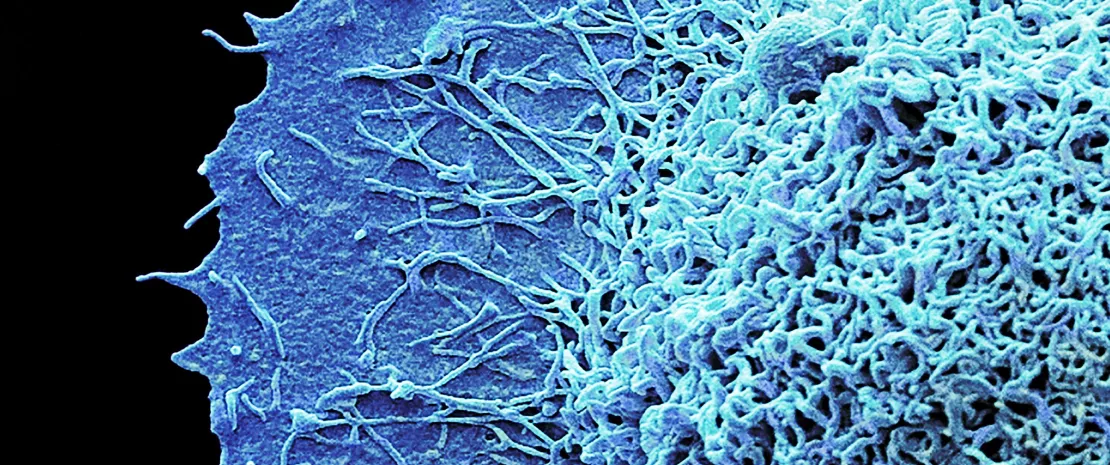
 Exposome: exposed microbiota puts health at risk
Exposome: exposed microbiota puts health at risk
 Microbiota and exposome: a dialog at the core of our health
Microbiota and exposome: a dialog at the core of our health