Medical research on the impact of antibiotics is hindered by the fact that the studies are generally carried out on polymedicated sick and hospitalized patients. As such, various confounding factors (infection, medications, hospital environment, potential immunosuppression) skew the observations.
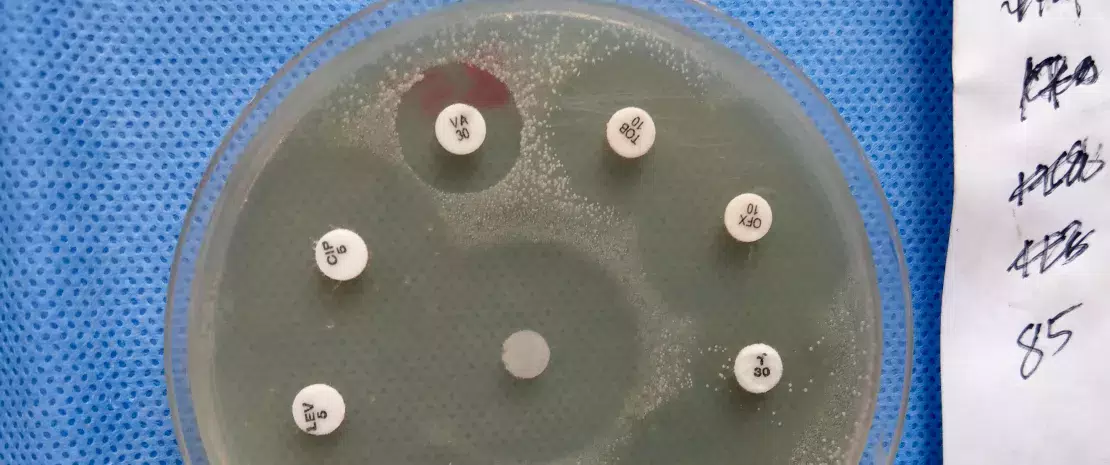
The only solution is to conduct prospective studies on healthy outpatient adults, such as this one. American researchers measured the impact of four antibiotic treatments, namely azithromycin (AZM), levofloxacin (LVX), cefpodoxime (CPD) or a combination of CPD and AZM), on the gut microbiota of 20 healthy volunteers randomized into four groups by collecting their stools before, during and two months after the end of treatment (15 collection points in all).
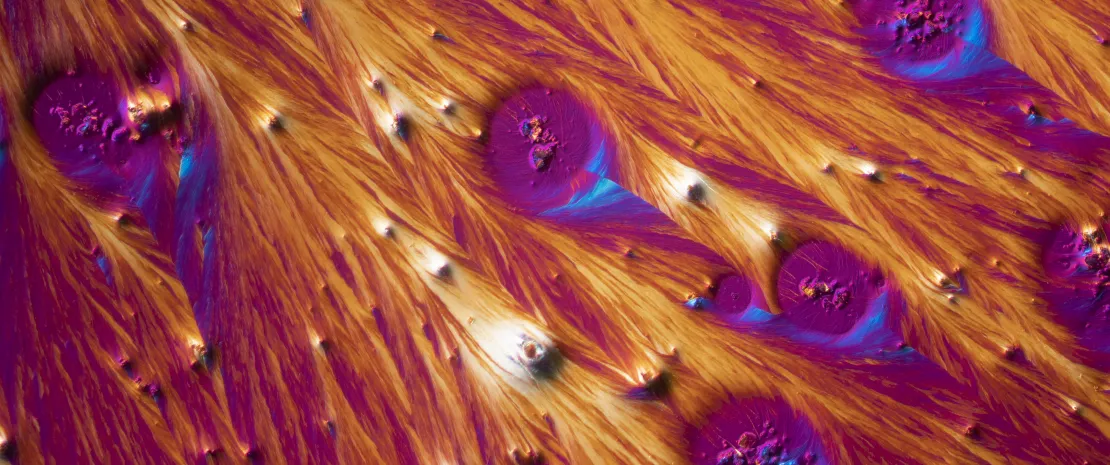
Antibiotic-induced gut dysbiosis
First finding: antibiotics reduce bacterial abundance and diversity. Depending on the treatment received, changes in abundance differed :
- higher levels of both Bacteroidetes and Clostridium for patients receiving CPD or CPD + AZM at Day 6,
- higher levels of Firmicutes, such as Eubacterium, Ruminococcus and Anaerostipes, for those receiving LVX or AZM.
In addition, AZM (alone or in combination), which has a long half-life, delays the recovery of bacterial abundance, eight bacterial species and some associated metabolic pathways compared to other antibiotics.
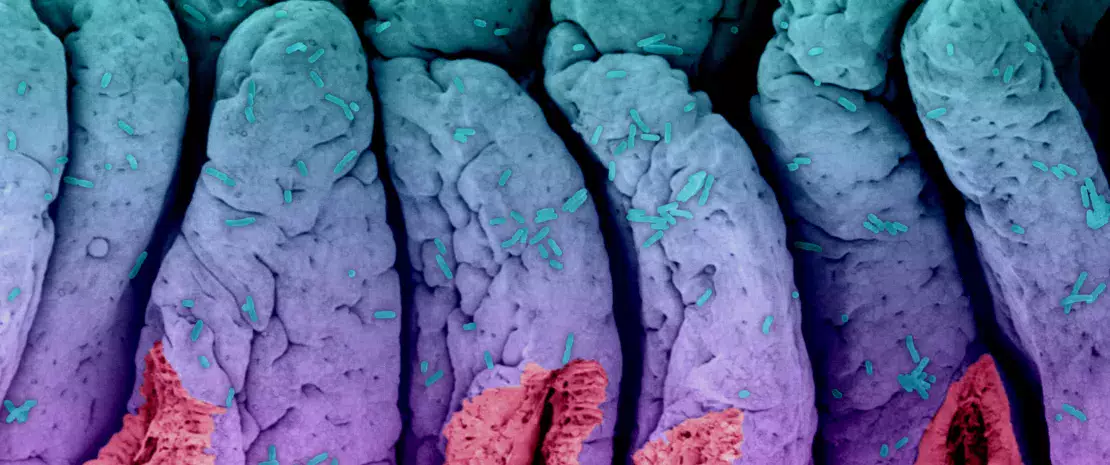
A reservoir of resistance genes
Another effect of the antibiotics was the emergence of a long-lasting reservoir of resistance genes in volunteers receiving CPD, AZM and CPD+ AZM treatments, in contrast to those receiving LVX. However, more importantly, the altered composition of their resistome would lead to an increase in three genes (tetO, cfxA, and tet40), two of which do not confer resistance to the antibiotics administered.
Consequently, antibiotic disruption appears to create opportunities for bacteria with broad resistance. For example, Bacteroides that survive CPD treatment, probably via ß-lactam resistance gene cfxA, would create a low-diversity, high-Bacteroides environment, favourable to pathogens such as Enterobacter. Short courses of antibiotics could trigger the acquisition or entrenchment of diverse resistance genes.
 The Janus face of Antibiotics: Life Savers and Microbiota Disruptors
The Janus face of Antibiotics: Life Savers and Microbiota Disruptors
 Impact of antibiotics on the gut microbiota, does it matter?
Impact of antibiotics on the gut microbiota, does it matter?