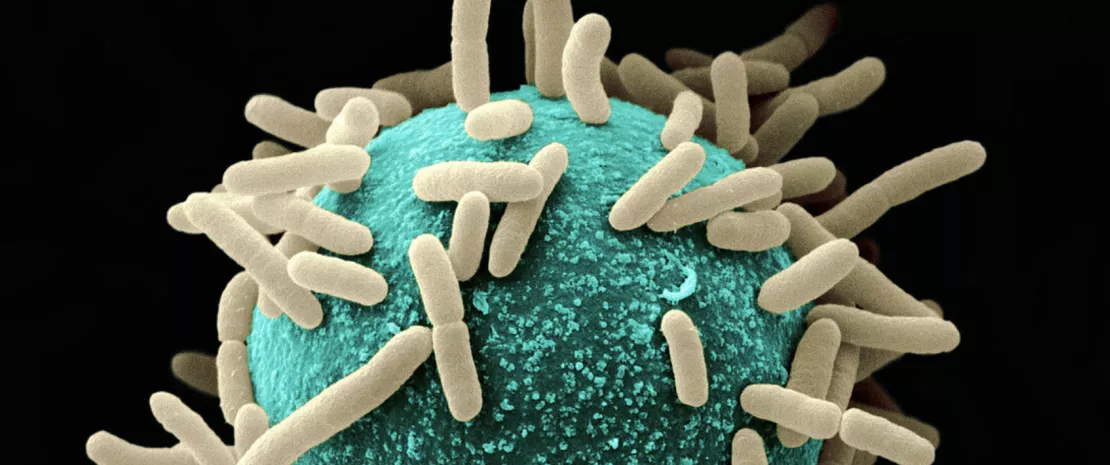
Can your gut microbiota predict the effectiveness of the Covid vaccine?
A new study has shown that certain characteristics of the gut microbiota may predict the level of Covid antibodies six months after vaccination. A first!

Tell me what your microbiota looks like, and I’ll tell you how the Covid vaccine protects you.
That’s the takeaway from a study 1 published last September in the academic journal Signal Transduction and Targeted Therapy.
The researchers succeeded in demonstrating that the presence of certain bacteria and molecules in the gut prior to the first injection may reinforce the immunity conferred by the vaccine, thereby extending its duration of action.
A promising avenue for the development of new adjuvants.
- 161 participants
- two Covid-19 vaccines
- six months follow-up
This finding was made thanks to the participation of 161 volunteers enrolled for six months.
121 participants received two injections of Comirnaty, Pfizer-BioNTech’s mRNA vaccine, while the remaining 40 received CoronaVac, Chinese firm Sinovac Biotech’s inactivated virus vaccine. No volunteers were infected with Covid during the study. Immediately prior to vaccination, then one month and six months later, the researchers took the following samples from the participants:
- blood samples to measure antibody concentrations;
- stool samples to identify the bacteria in their gut microbiota and measure the levels of substances produced by the subject and their bacteria (vitamin B3, GABA, fumaric acid, etc. – i.e., the renowned “metabolome”).
The researchers found, first of all, that Comirnaty achieves better immunity than CoronaVac.
How do vaccines work?
To defend yourself effectively against disease, you need to know the enemy. This is what vaccination against viruses is all about:
- First, an antigen is injected into your body, i.e., an inactivated or weakened pathogen or a fragment of it;
- Your immune cells produce specific antibodies that target this antigen;
- Your body then stores “memory” cells;
- When infected by the true pathogen, activation of your immune system’s memory cells is swift and effective (more so than when the body discovers the pathogen for the first time);
- The pathogen is destroyed.
Produced from the inactivated SARS-CoV-2 virus, CoronaVac operates on this principle. Comirnaty is a little different: it contains a sort of “blueprint” (the famous messenger RNA) that enables cells to manufacture proteins identical to those present on the surface of the Covid virus. These proteins then play the role of antigen for the manufacture of antibodies.
Source: WHO 2
State of gut flora modulates vaccine-induced immune response
In the Comirnaty group, patients whose gut microbiota before the first injection was abundant in bacteria such as Bacterium adolescentis,
(sidenote:
Bifidobacterium
A genus of Y-shaped bacteria, most species of which are beneficial to humans. They are found in the gut of humans, and in some yogurts.
They:
- Protect the gut barrier
- Participate in the development of the immune system and help fight inflammation
- Promote digestion and improve symptoms of gastrointestinal disorders
Sung V, D'Amico F, Cabana MD, et al. Lactobacillus reuteri to Treat Infant Colic: A Meta-analysis. Pediatrics. 2018 Jan;141(1):e20171811.
O'Callaghan A, van Sinderen D. Bifidobacteria and Their Role as Members of the Human Gut Microbiota. Front Microbiol. 2016 Jun 15;7:925.
Ruiz L, Delgado S, Ruas-Madiedo P, et al. Bifidobacteria and Their Molecular Communication with the Immune System. Front Microbiol. 2017 Dec 4;8:2345.
)
bifidum and Roseburia faecis had higher levels of SARS-CoV-2 antibodies in their blood six months later. The same type of stronger, longer-lasting immunity was found in those with a metabolome richer in vitamin B3 and GABA.
The gut microbiota
In the CoronaVac group, a low abundance of Faecalibacterium prausnitzii and a higher abundance of Phocaeicola dorei – a signature found in Covid-infected patients – was associated with better immunity at six months, as was a higher presence of fumaric acid in the metabolome, a compound known to hinder virus replication.
Another finding was that, for the Comirnaty group, a greater proportion of the bacterial strains in the microbiota altered by the vaccine had not recovered their pre-vaccination state when compared with the CoronaVac group. While it remains difficult to analyze the consequences, the researchers point out that some of the strains affected are the same as those found altered in people suffering from long Covid.
Towards the development of new adjuvants
We already knew that microbiota, genetics, and body weight influence the efficacy of Covid vaccines. However, this is the first study to show that the structure of the microbiota and metabolome prior to vaccination can predict the level of immunity six months later.
While these results must be confirmed by a more targeted study, they suggest that it will soon be possible to use bacteria or metabolome compounds as adjuvants to improve vaccine efficacy.